Can COVID help accelerate universal health coverage progress?
The world has been celebrating Universal Health Coverage (UHC) Day for seven years now. But ahead of this year’s UHC Day on December 12, I am pausing to reflect on what our shared COVID-19 experience means for our journey to achieve universal health coverage globally.
COVID has revealed weaknesses in every country’s health system. It has challenged governments to organize an emergency response, and simultaneously maintain essential health services — especially for the most vulnerable. These domestic system weaknesses contribute to global vaccine inequity when donated or procured vaccines can’t be delivered quickly, exacerbating COVID’s impact, enabling the rise and spread of new variants, and ultimately extending the life of this pandemic. System weaknesses also mean that COVID is derailing previous progress, leading to backsliding in areas like routine immunization and child survival.
Even as we strive for global solidarity around a common viral enemy, the pandemic accentuates how much all countries need strong domestic leadership of their own health systems — and this has accelerated the long overdue localization movement in global health.
While fully recognizing the tragedy that continues to unfold — and all the work we have ahead — I feel somewhat optimistic as UHC Day approaches…because this pandemic makes the case for UHC. It strengthens our resolve to ensure that every country’s health system is stronger and more resilient than ever. And all the current attention to defeating COVID — if we harness it well — offers potential for lasting health systems change.
But what exactly do strong health systems look like? And how can the global health community support countries around the world to strengthen them…especially at this moment when health systems are in the spotlight?
Today, we might be tempted to equate a strong health system with vaccine delivery and access to oxygen for people in respiratory distress, just as 10 years ago we often equated strong health systems with their ability to diagnose HIV/AIDS and distribute antiretrovirals. Those are all part of any strong health system.
But I’d like to suggest we think about strong health systems in a different way, especially if we want to prepare for the next unknown global health shock and make progress on a broad range of health priorities that may not be top-of-mind right now.
At Results for Development (R4D), we define a “health system” as the people, inputs, institutions, policies and processes within a country — and how they interact to deliver high-quality, affordable health care for all.
We try to make this more concrete by describing what a strong health system looks like in practice. We believe strong health systems are marked by their ability to:
- Deliver high-quality services and essential medicines equitably to the whole population, for the long-term.
- Mobilize and coordinate resources to solve priority challenges.
- Work in a coherent way to achieve desired health outcomes.
- Measure results.
- Innovate, learn and adapt.
- Be accountable and responsive to citizens and trusted by them.
- Be resilient to shocks and capable of adapting to changing circumstances.
This description does not list all the important nuts-and-bolts components of health systems — like well-trained clinicians, adequate supplies of drugs, comprehensive information systems, and financial flows that ensure affordability for all. Rather, it focuses on important capacities that enable response, adaptation and continuous improvement — which are the foundation for successful systems change efforts and resilience during challenging times.
So, how can development partners support countries to achieve strong health systems?
We often mobilize support to country leaders to help them address an immediate health system challenge like maternal mortality or one component of a health system like primary health care, bringing strong evidence-based approaches. Right now, many of us are supporting countries with aspects of their COVID response.
But how we go about our work can have a tremendous effect — either positive or negative — on whether the country’s health system actually gets stronger as a result of our efforts, rather than merely achieving a desirable short-term output.
Here are 5 ways we can support countries to achieve strong, resilient health systems
- Let country leaders lead. It should go without saying, but true and lasting change doesn’t happen when external stakeholders are at the helm. Local leadership has often been undermined, with years of externally-led interventions and the resulting power imbalance between donors and country leaders. But development partners can shift our approach. We can play a supporting role to create the conditions for local leadership to succeed — providing global evidence that can be adapted to inform local decision-making and connecting leaders from different countries to share their experiences, learn best practices and co-develop solutions. We can support current and emerging leaders to play their role more effectively and work more inclusively with stakeholders across the health system and other sectors.
- Support the institutionalization of domestic diagnosis and solution generation. Those of us who bring a birds-eye view of global evidence and experience across multiple countries are certainly helpful thought partners in health systems strengthening, but only if we stand back and allow domestic leaders to diagnose root causes and co-create solutions built on local and global evidence and diverse local stakeholder input. This leads to solutions that are contextually appropriate and operationally feasible. And when these kinds of processes get institutionalized, the health system becomes stronger and more capable of solving the next problem.
- Encourage inclusive change processes. Health system strengthening is deeply political. Let’s stop pretending that a technical solution is enough. Solutions to complex health system challenges require robust consultation and communication processes that involve diverse stakeholders, such as patients, clinicians, and advocates and the associations that represent them. Many stakeholders across different levels of government, civil society and the private sector must be involved and supportive to ensure strong implementation of solutions. As development partners, we can either support or hinder these inclusive processes. When we focus too much on quickly delivering an output, we undermine the inclusive processes that are necessary to strong health systems.
- Encourage holistic thinking about the interrelated components of the system, while making progress on immediate priorities. When we are trying to solve an immediate challenge, it’s natural to focus on that symptom and address it quickly and directly. The narrow way global development projects are structured often reinforces this inclination. But, in strong systems, different components of the system must operate coherently to achieve a goal. For example, financing incentives must reinforce delivery objectives. As we support countries to delivery COVID vaccines, develop oxygen supply chains, and create stronger disease surveillance systems, we should encourage thinking beyond the silo of an individual component of the system to ensure system coherence.
- Support implementation efforts underpinned by continuous improvement and adaption. Rarely does a program or a solution work perfectly when first implemented. Strong health systems assess the effectiveness of new programs or interventions quickly, and then use that analysis to learn and improve or pivot when necessary. And strong health systems institutionalize this kind of continuous improvement through routine measurement and use of data for adaption, iteration and improvement.
These approaches support country leaders to drive systems change. And following them is one way we can act on donors’ and implementing partners’ commitments to locally-led development with stronger resolve.
A helpful framework to support your own health systems strengthening efforts
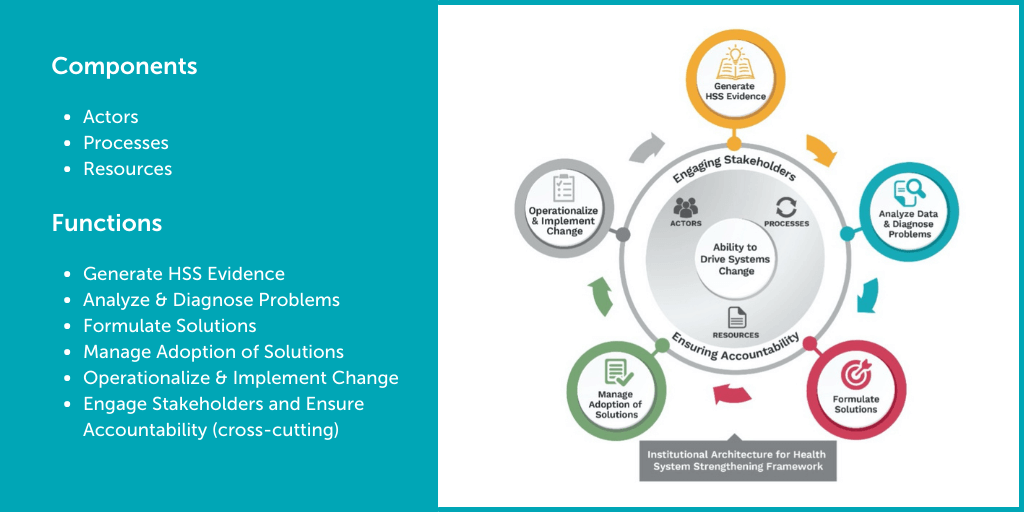
If you are a health system leader or a development partner interested in how to create stronger, more resilient health systems, check out this framework for improving the institutional architecture for health systems strengthening (see Figure 1 below). It defines the six functions that produce health system changes and the actors, processes and resources that must work together to perform these functions.
Figure 1: Institutional Architecture for Health Systems Strengthening
My R4D colleagues and our partners who lead the Health Systems Strengthening Accelerator, an initiative funded by USAID and the Bill & Melinda Gates Foundation, developed this approach to complement other health system frameworks. It focuses on concrete ways to strengthen a country’s ability to drive health system change over time. This framework can be used alongside COVID response activities, to ensure our efforts to address immediate challenges also yield stronger health systems for the long term.
The framework has also informed our recently launched R4D strategy, which emphasizes working in a way that promotes (and does not undermine) local leadership. Every time we engage with a country — bringing technical expertise and evidence to help solve an immediate challenge — we also aim to support the institutionalization of capacities to drive systems change that will help local leaders address the next challenge.
***
UHC Day promotes progress on what will be a decades-long global journey toward comprehensive universal health coverage. This requires strong health systems capable of driving change.
Right now, global and country-level leaders are focused on addressing the challenge of our generation — managing the COVID-19 pandemic. In meeting this moment, the international community stands to gain and learn a lot. If we go about our COVID response efforts in a way that strengthens health system resilience and capacity to change, I am optimistic we will harness this moment to accelerate global progress toward UHC.
Photo © World Bank/Henitsoa Rafalia