Stories like Dyah’s — marked by complications, uncertainty, and a lack of consistent support — are all too common. While many women survive high-risk pregnancies, too many do not. And Indonesia continues to face one of the highest maternal mortality rates in Southeast Asia, with 189 deaths per 100,000 live births (2020 Population Census).
Despite expanded health coverage under the national insurance scheme, critical gaps persist in the quality and accessibility of maternal and newborn health services. Many health facilities lack the incentives or capacity to follow national service standards, and outdated payment mechanisms have discouraged comprehensive care, especially at the primary level. High hospital costs driven by emergency referrals have underscored the need to shift more services to frontline health centers.
To tackle this, the Indonesian Ministry of Health and the National Health Insurance Agency, in collaboration with Results for Development (R4D) and ThinkWell, piloted new purchasing arrangements for maternal and newborn health, with additional support from Gadjah Mada University as the evaluation partner.
R4D facilitated a multi-stakeholder process to diagnose service delivery challenges, developed a viable pilot design, and played a central role in implementing interventions. This included strengthening and improving the efficacy of monitoring systems, supporting evaluation and implementation research, and leading efforts to strengthen institutional capacity.
The pilots, which were implemented in Kota Serang and Kabupaten Serang between 2022 and 2023, introduced both strategic purchasing and service delivery reforms. These included updating benefits packages, linking payments to specific quality standards, and improving access to health services at private clinics. Other systems strengthening strategies were equally important: coordination across government institutions was improved through monthly meetings, electronic claims systems, and joint monitoring; capacity was built via on-the-job training; and consistent evaluations were carried out to ensure quality improvement.
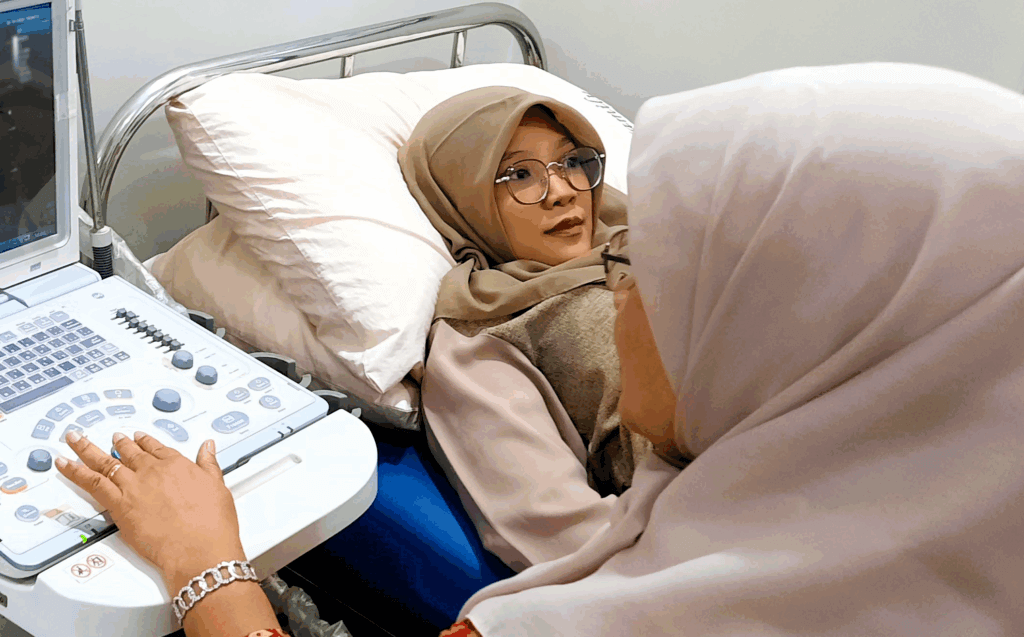
Dyah’s public health facility was one of several selected to participate in the pilot program. As a result, the facility was better equipped, and providers were better supported. Facilities received timely payments for delivering key services, including services essential for managing high-risk pregnancies, such as ultrasounds and screenings for high-risk conditions like preeclampsia. And the training that midwives and other health workers received helped them deliver care in line with national standards. For Dyah, this made all the difference.
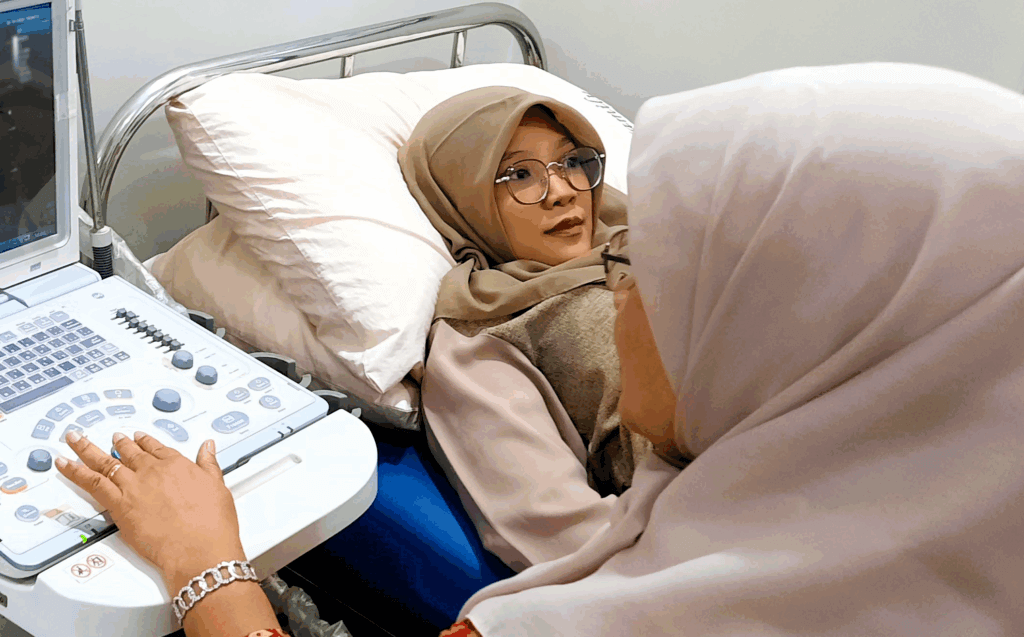
Expectant mother receiving an ultrasound examination.