Improving access to malnutrition treatment within primary health care
An opportunity not to be wasted
[Editor’s Note: This is the first post in a blog series on sustainable strategies to improve access to wasting treatment. The series was spurred by the historic half a billion dollars pledged by donors this year to improve child nutrition, with an aim to review strategic ways to use this funding. Insights highlighted are based on a resource guide developed by R4D and UNICEF that offers an easy-to-follow process for governments to identify integration actions that can help achieve program goals for the early detection and treatment of child wasting within routine primary health care systems.]
Progress to reduce the burden of child wasting has been significant over the last two decades: the number of children with severe wasting has decreased while the number of children accessing treatment has increased. However, only 1 in 3 children with severe wasting are reached with timely treatment, leaving an estimated 9 million children left untreated at any point in time. On top of this, today we face a crisis-on-top-of-crisis situation where conflict, climate change, COVID, and unstable food prices have together drastically increased the risk of malnutrition, particularly among vulnerable groups.
In July and September of this year, donors pledged $577 million to tackle severe wasting and improve child nutrition. While much of this is targeted to humanitarian support, the historic investment made by global health leaders presents an opportunity to make sustainable change and strengthen primary health care (PHC) services to improve nutrition and save lives in the long term.
Why does this matter for PHC performance?
Contrary to common belief, most children with severe wasting do not live in emergency settings. As USAID Administrator Samantha Powers noted at the recent United Nations General Assembly, “nearly two-thirds of children who need treatment live in places who don’t normally receive humanitarian aid.” The condition is no different from any other disease where these children and their caregivers rely on their PHC system in times of need. When left unidentified and untreated, it is a failure of the health system.
Without early identification and treatment, children with severe wasting are at a heightened risk of mortality and health complications that may be difficult to respond to in an already overwhelmed health facility. In fact, one of the most vulnerable groups — children with wasting, stunting, and who are underweight — have a 12-times increased risk of mortality compared to their healthy counterparts.
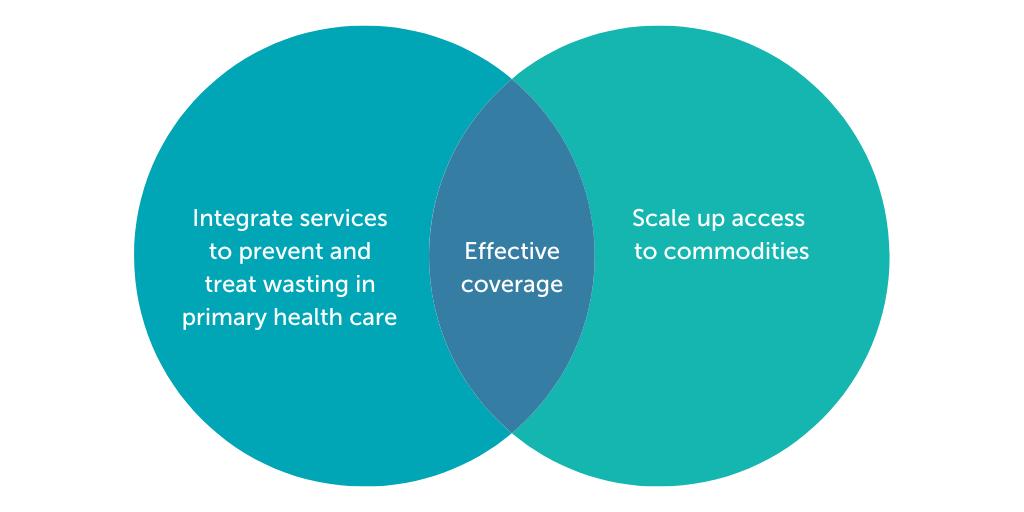
Identifying severe wasting as early as possible reduces the risk of complications, and, in turn, additional pressure on the PHC system. Ensuring children with severe wasting are treated reduces the risk of mortality. To achieve sustainable and effective coverage of wasting treatment, integrating the early detection and treatment of child wasting and scaling access to ready-to-use therapeutic food are critical (Figure 1). Integration is a strategic process in which vertical services are embedded into broader child health programs or systems, and the responsibility on the part of national governments is increased while reducing reliance on external support. Integration can increase the coverage and equity of services (for screening and treatment), reduce costs and increase efficiency of programs, and increase programmatic and financial sustainability.
Figure 1: Components for effective coverage of wasting treatment
The UNICEF and R4D resource guide on the integration of early detection and treatment of child wasting into PHC services discusses strategic actions governments can take to embed these services into existing health platforms. The government of Ethiopia has been a leader in scaling up wasting treatment over the last few decades and has recently drafted their own national integration plan. Later this year, stakeholders across regions are coming together to validate the plan and develop their own subnational operational plans. An upcoming blog in this series will share lessons learned from this process.
A unique opportunity to strengthen health systems to improve wasting
Even though some of the pledges made in July and September are time-bound, such as USAID’s massive pledge of $200 million to be disbursed within one year, country governments and development partners need to come together to ensure investments made today last into the future. But what must be done to ensure this influx of funding can be sustained in the long term?
Strategic investments are necessary to make sustainable changes across the health system

In this blog series, we will explore sustainable strategies to improve access to wasting treatment within the health system. We want to start a discussion on how to catapult programs to success by discussing what kind of investments are needed in the system and where.
Over the course of the next few months, we will introduce concepts of integration across health system building blocks and investigate how funding can be prioritized to ensure long-term impact. Using the wasting integration resource guide as a framework, we will explore the following key questions:
- How to strengthen primary health care services to efficiently deliver essential nutrition actions and wasting services?
- How to ensure health information systems provide accurate and timely data on child wasting? burden and treatment, for use in decision making on where to allocate resources or send RUTF?
- How to ensure a sustained, predictable, and continuous supply of RUTF to meet growing demand?
- What have we learned from Ethiopia’s process of developing their national integration plan and how can this experience translate to other contexts?
Strategic investments are needed to improve PHC performance across each of these areas. The intention of this series is to spark conversation on how this unprecedented investment of over a half billion dollars can be used. Together, let’s ensure that in 10 years, the year 2022 is marked not as a devastating year for malnutrition, but as a pivotal year when sustainable access to treatment became possible for all children in need.
Photo © Kate Consavage/USAID
Catch up on the series
- Improving access to malnutrition treatment within primary health care
- Strategic opportunities to scale ready-to-use therapeutic foods
- Optimizing primary health care to treat child wasting
- How the Philippines integrated malnutrition management into its health system
- Q&A: Strategic approaches to improve access to wasting treatment in Ethiopia













