Optimizing primary health care to treat child wasting
[Editor’s Note: This is the third post in a blog series on sustainable strategies to improve access to wasting treatment. The series is spurred by the historic half a billion dollars pledged by donors this year to improve child nutrition with an aim to review strategic ways to use this funding. Insights highlighted are based on a resource guide developed by R4D and UNICEF that offers an easy-to-follow process for governments to identify integration actions that can help achieve program goals for the early detection and treatment of child wasting within routine primary health care systems. This blog aims to answer the key question: How can we strengthen primary health care services to efficiently deliver essential nutrition actions and wasting services?]
Child wasting is the deadliest form of malnutrition, responsible for 1 in 5 deaths among children under 5. The problem is widespread and rising in countries across regions, and not just countries facing humanitarian crises. Some countries have even seen an increase in child wasting by more than 40%. However, child wasting is preventable and treatable.
The UN Global Action Plan for Child Wasting (GAP), a framework for accelerating the prevention and management of child wasting, calls for countries to increase the coverage of treatment services for children with wasting by 50% by 2025 including through strengthening health systems and integrating treatment into primary health care (PHC) services. This blog describes several actions to integrate screening and treatment into PHC services.
How is screening and treatment currently implemented within the health sector?
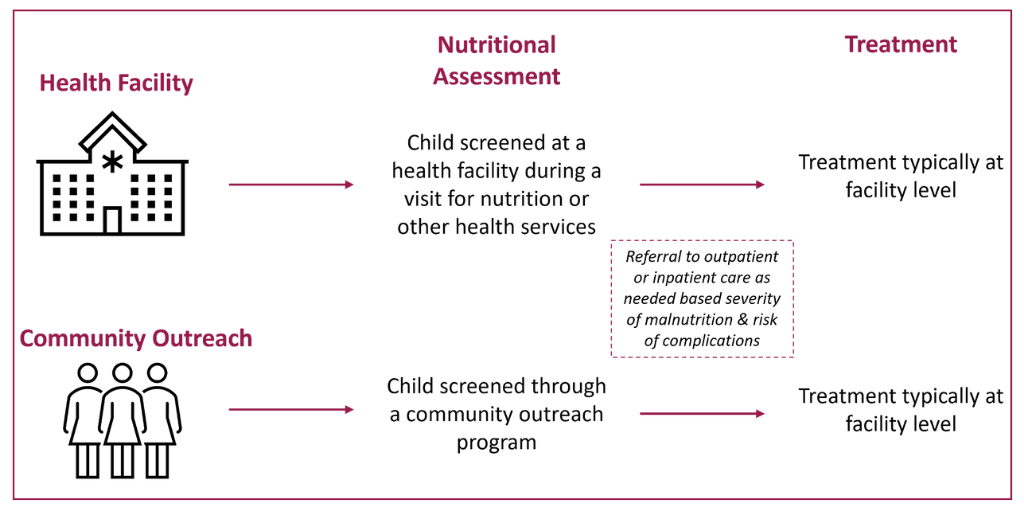
Screening for child wasting within PHC services is critical to identifying cases early as this prevents complications and saves lives. A trained healthcare worker completes screening either during a visit to a health facility or site (e.g., a well-child visit, sick-child visit, or immunization visit) or through community outreach programs (Figure 1). Once nutritional status is assessed, children may be referred for inpatient or outpatient treatment, depending on the severity of malnutrition and presence of medical complications. Children with less severe cases and no medical complications typically can be treated with ready-to-use therapeutic foods (RUTF) in their own home, rather than a health facility.
Figure 1: Services required to prevent and manage wasting in the health sector
What are the current challenges to service delivery?
Figure 1 shows how screening for wasting and treatment integrated within the health system is intended to work. However, in most countries, wasting services are often provided in parallel to other child health services, including through delivery outside of government platforms. This results in fragmented service delivery and inefficiencies. There are several common constraints to service delivery, including –
- Community health workers (CHWs) are overburdened and often do not have time to screen for child wasting which leads to limited success of community outreach efforts
- Limited capacity of health staff to deliver wasting services which results in low treatment coverage at the facility level
- Siloed management of health services hinders joint programming efforts and leads to missed opportunities for efficiency gains to detect and treat child wasting
- Predictable and unpredictable surges in child wasting can overwhelm the health system’s ability to provide critical services (e.g., predictable due to seasonal changes, or unpredictable due to emergencies)
Additional constraints across health system building blocks affect service delivery, which are explored in the resource guide on Integrating Early Detection and Treatment of Child Wasting into Routine Primary Health Care Services.
How can PHC services reach more children with wasting treatment?
Integrating screening and treatment services into PHC can help ensure more children are reached with services and no child is missed. Figure 2 shows examples of integration actions to address the above constraints. Each action must be assessed based on feasibility and the risks and benefits to wasting services and PHC in each context.
Figure 2: Potential Integration Actions to Address Constraints
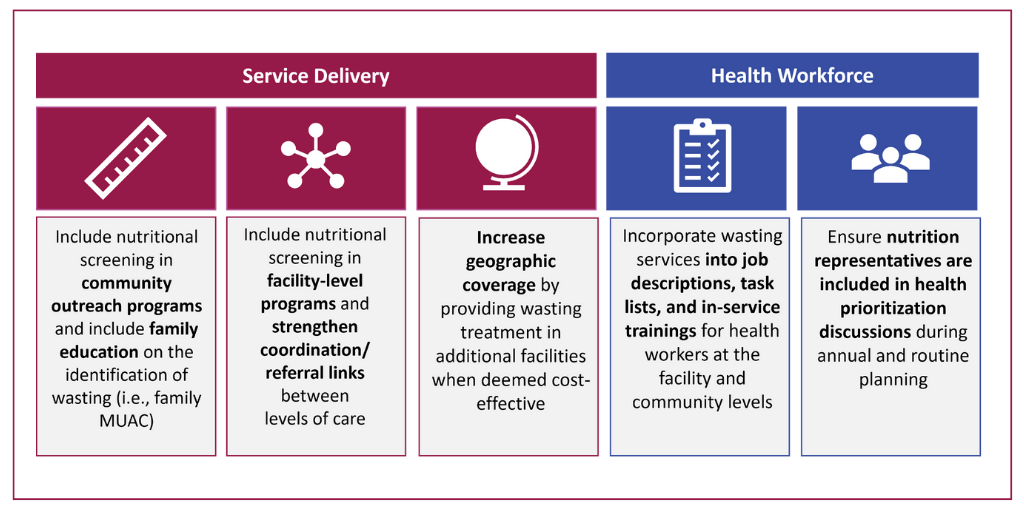
Integration actions can bring important benefits, including increased coverage and equity for wasting services, reduced costs and greater efficiency, and increased sustainability. Additionally, reducing some of the burden on the health system can ultimately result in an overall improved ability to meet the broader health needs of children.
How can simplified approaches offer even stronger potential for the PHC system to reach more children?
Many countries are also considering simplified approaches —alternatives to existing national and global protocols for the treatment of child wasting. Many of these simplified approaches are designed to reduce the burden on the PHC system by decreasing the number of complicated wasting cases and children requiring treatment in health facilities.
For example, one simplification includes the use of CHWs not only for the screening of wasting, but also for the treatment of wasting without medical complications at the community level within existing community outreach programs. This method can benefit the PHC system as children skip the referral step noted in Figure 1 which saves time and costs. It also reduces the burden on caregivers as treatment is more accessible, increasing the likelihood the child will receive the full course of treatment and incur fewer complications. Several countries, including Angola, Bangladesh, Ethiopia, India, Malawi, Mali, Niger, Pakistan, Senegal, South Sudan, and Togo, have piloted treatment by CHWs with improved outcomes. The growing evidence base for this simplified approach generally shows the method to be as effective as facility-based treatment, with the added benefits noted above.
To learn more about other simplified approaches and resources available please refer here.
Well-designed integration actions can help governments and partners to save more lives
Integrating early detection and treatment of child wasting into routine primary health care services can reduce burden on the health system, improve overall child health, and help save the lives of millions of children who experience wasting. The resource guide can be used as a tool for governments and their partners to identify the integration actions that make the most sense for their context by following the six steps in the process. By doing so, this can generate clear plans for all partners to follow.
Photo © Russell Watkins/DFID
Catch up on the series
- Improving access to malnutrition treatment within primary health care
- Strategic opportunities to scale ready-to-use therapeutic foods
- Optimizing primary health care to treat child wasting
- How the Philippines integrated malnutrition management into its health system
- Q&A: Strategic approaches to improve access to wasting treatment in Ethiopia













