Launching a strategic purchasing assessment in Ethiopia
Where do we go from here?
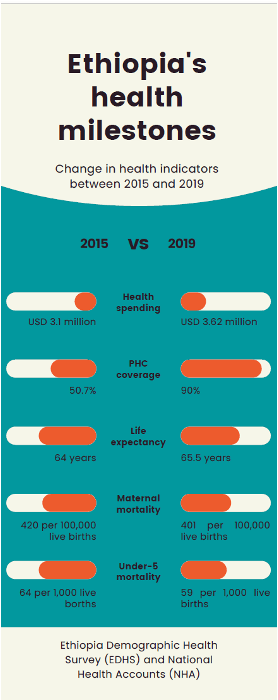 In the past two decades, Ethiopia has achieved significant milestones in improving health indicators. These achievements are credited to increased prioritization by the Government of Ethiopia in increasing resources for health, and creating bold strategies through the Health Sector Transformation Plans I and II.
In the past two decades, Ethiopia has achieved significant milestones in improving health indicators. These achievements are credited to increased prioritization by the Government of Ethiopia in increasing resources for health, and creating bold strategies through the Health Sector Transformation Plans I and II.
Through these strategies, Ethiopia prioritized primary health care (PHC) access, increased resources to health providers, expanded provider autonomy to use these resources according to local priorities, defined a benefits package through a participatory process, implemented a broad exemptions program, introduced community based health insurance (CBHI) to expand access to health services while providing financial protection against health spending, and legislated the creation of the Ethiopia Health Insurance Service (EHIS) to develop the health insurance system in Ethiopia. Through systematic and deliberate actions led by the Federal Ministry of Health (MOH), and support from partners, Ethiopia has created a healthier nation to further its economic growth.
Despite these gains, there are challenges that persist. For example, public spending on health per capita remains low at $36.3 (2019) and attempts to raise domestic resources for health have been constrained due to fiscal space. Ethiopia benefits from external funding channeled to priority health programs through on-budget and off-budget resources that contribute 34% of total health expenditure (2019).
As Ethiopia’s economy grows, and as the global financing of health programs declines, there will be an expectation to increase resources for health. Against the backdrop of limited fiscal space, a decline in donor financing, and increased demand for health services, the government and other stakeholders are looking to address how Ethiopia can use limited resources better. This could include efficiency gains in how services are delivered and improving how resources are allocated and used across the health system — which are areas that can be addressed by the purchasing function of health financing systems.
As a member of the USAID’s Health Financing Improvement Program (HFIP) consortium, R4D provides technical support to the Ethiopian government and other stakeholders to improve how funds flow through the health system — and how they are used. This includes supporting evidence generation, facilitating technical and policy dialogues. R4D is also supporting efforts to explore interventions to increase domestic resource mobilization, introduce strategic purchasing mechanisms, improve efficiency in use of health resources, and provide financial protection for the most vulnerable.
Through their broad and deep involvement in health financing, the HFIP consortium initiated discussions with EHIS on how best purchasing can be improved in Ethiopia. To further these discussions, the consortium facilitated and brokered EHIS engagement with the Strategic Purchasing Africa Resource Centre (SPARC) to assess the purchasing function of Ethiopia’s health financing schemes to understand the opportunities for improvement and gain “more health” from available resources.
This request was within the mandate of EHIS to improve the function of the health insurance system in Ethiopia. EHIS led the technical working group tasked with providing oversight to the assessment, in collaboration with MOH, Ethiopian Pharmaceuticals Supply Service, Clinton Health Access Initiative, HFIP and SPARC. The strategic health purchasing progress tracking framework — co-developed by SPARC and African partners and applied in 10 countries — was used as the data collection and analytical framework for the assessment. Key findings from the assessment are documented in this report and summarized in this brief.
In this blog, we summarize key insights and reflections from a panel during the dissemination of the assessment report in November 2022.

From L-R: Leulseged Ageze (Chief of Party USAID-HFIP), Dr. Muluken Haile (Deputy Director General EHIS), Dr. Feven Girma (Director MOH Partnerships and Cooperation Directorate)
Launch of the “Strategic health purchasing in Ethiopia: an assessment and strategic actions to improve purchasing” Nov. 19, 2022.
Ethiopia has made significant progress in purchasing
Across all the dimensions of the framework, Ethiopia has made gains in creating a regulatory framework that provides purchasers with the mandate to carry out purchasing functions at various levels of government. Purchasers set budgets at the beginning of the fiscal year for their operational costs and for implementing core purchasing functions. Public facilities have autonomy to use internally generated revenue (user fees) and reimbursements from CBHI. The benefit packages are based on the Essential Health Service Package (EHSP) that broadly cover population health needs. Purchasers are testing capitation and performance-based financing to improve inherent challenges with the fee-for-service and input-based budgets which are used predominantly in Ethiopia. Systems exist to monitor provider performance based on routine data collection and reporting through the DHIS2 platform and monitoring mechanisms for service delivery indicators.
But there is a sizable strategic purchasing agenda that needs to be addressed
1. The governance framework exists but implementation needs to be enhanced.
Ethiopia has a strong governance framework that clearly defines the mandate of the MOH, Regional Health Bureaus (RHBs), CBHI woreda schemes and EHIS. Some of the roles that require strengthening are the EHIS as the purchaser of tertiary healthcare services on behalf of the CBHI schemes, while woredas remain the purchasers of primary care using output based provider payment methods; capacity building of providers to fully utilize the autonomy provided in public financial management regulations; the MOH aligning the program-based budgeting process to regional budgeting processes, and linking better the budgeting process to performance and achievement of objectives of the health system.
2. Broad exemption policies create financing constraints at facility level.
There are 1018 interventions included in the EHSP. Cost sharing policies identify 570 interventions as exempt with the remaining interventions listed for cost sharing and cost recovery. Because there’s no clearly defined funding stream for the exempted services, these interventions are provided within the resource envelope providers generate through user fees and external resources. This creates funding constraints at provider level impacting the quality of care they provide. The MOH is addressing this by developing a mechanism for financing exempted services and has already established a technical working group to review the cost of interventions which are said to be exempted, the total budget needed to cover them, and possible funding mechanisms.
3. Contracting arrangements are at nascent stages but need further strengthening.
There are loose agreements between purchasers and providers, and a lack of clear accreditation and contracting instruments to inform the selection of providers and to support quality assurance of service delivery.
4. Provider payment lacks incentives for high quality care.
The dominant payment methods in use are fee-for-service and line-item budgets. Line-item budgets are based on historical expenditure for inputs such as staff, medicines, and commodities. The fee-for-service user fee schedule is set by the MOH, RHBs or facility boards. CBHI pays providers using these fee-for-service schedules. The mix of provider payment methods currently in use does not give incentives to providers for efficiency or quality. Lessons generated through the capitation and performance-based financing pilots may improve design of provider payment to provide the right incentives throughout the health system.
5. Performance monitoring systems are not used as expected, to inform purchasing decisions.
Routine data collection and reporting processes exist, but these are not used to provide feedback for improvement or carry out system-level analysis of utilization and quality to inform purchasing decisions.
What’s next?
Ethiopia has been proactive in addressing some of these shortcomings. For example, the EHIS is revising the health insurance benefit package to better define “what to buy” through pooled funds from the CBHI, and MOH has initiated a mechanism for financing exempted services. Further improvements needed to improve strategic purchasing in Ethiopia as highlighted in the assessment report include:
- Clearly defining the roles and responsibilities of all purchasing agencies to resolve conflicts and overlaps, while ensuring adequate lines of accountability for strategic purchasing
- Ensuring that adequate resources and effective purchasing mechanisms for PHC take precedence over efforts to develop complex provider payment methods for secondary and tertiary-level care
- MOH to finalize and implement the financing modality for exempted services.
- Developing a guideline for contracting arrangements and engaging public and private providers. This includes defining accreditation standards for the selection and inclusion of providers and creating a framework to engage and contract private providers
- Developing a clear performance monitoring strategy that incentivizes good provider performance and good-quality care and integrates and builds on existing platforms to create an integrated national platform
- Build on existing information systems to support the design of more complex provider payment systems over the long term
Ethiopia has made remarkable gains in improving access to health care, as evidenced by increased access to primary care and declines in infant and maternal mortality rates. Although more public funding is needed to further increase access to high quality health services and achieve universal health coverage (UHC), more can be done within the current financial envelope by improvements in strategic purchasing.
There are no magic bullets.
Strategic purchasing is a journey, and everyone needs to work together. Ethiopia has clear next steps to continue this journey, working with like-minded partners to continue to make progress toward strategic purchasing and the ultimate goal of UHC.
Additional Resources
Photo © USAID/Amy Fowler













