Principles for integrating nutrition services into routine primary health care
As mothers of young children, it’s hard to accept that in 2021, 45 million children worldwide experience wasting (a form of acute malnutrition where children are too thin for their height).
It’s even harder to accept that only 1 in 3 of these children receives the care they need to survive and thrive. This situation has been exacerbated by the COVID-19 pandemic — due to the economic hardships households face which result in food insecurity and health system disruptions.
But there’s a way forward with proven approaches to address the problem through the early detection and treatment of child wasting, which can help save lives.
Twenty years ago, this started as the community-based management of acute malnutrition (CMAM) approach, which was shown to be extremely effective to bring wasting treatment closer to the children who need it. Since then, many countries have begun integrating the treatment of child wasting into their routine systems.
However, more often than not, these programs are still delivered through emergency and humanitarian relief settings — despite the fact that child wasting is an endemic issue in many places that must be addressed in a more holistic way.
All UN agencies working on nutrition came together in 2020 to release the UN Global Action Plan on Child Wasting to accelerate joint actions toward the achievement of the 2030 SDG Goal of less than 3% of children globally affected by wasting. The integration of wasting services within primary health care (PHC) is core to the GAP framework to improve coverage and increase access to treatment for wasted children.
Integrating the early detection and treatment of child wasting within routine primary health care services is critical to universal health coverage (UHC).
Some countries — like Ethiopia — are much farther along in this journey. Others are not sure where to begin. There are also some misconceptions about what “integration” means.
To better support countries in increasing access to services for the care of child wasting, R4D and UNICEF co-developed practical materials for national health sector leaders — Integrating Early Detection and Treatment of Child Wasting into Routine Primary Health Care Services: A Resource Guide to Support National Planning. This was developed through a consultative process with country governments, development partners, and experts in health systems strengthening and nutrition.
Just as we want our health systems to support our children’s healthy growth, this guide is intended to support all national governments and key stakeholders to bring critical nutrition services closer to those who need it the most.
Through this process we identified several guiding principles for the approach to follow:
- All services required to prevent and manage child wasting across multiple sectors should be considered with an integration lens. While the guide focuses on nutrition within PHC, services to prevent child wasting are required alongside early detection and treatment across the food system, health, social protection, and WASH systems.
- Integration is context dependent and can take various forms. The current state of integration varies widely across countries along the two dimensions used to define integration in the guide — which are, first, the extent to which services are embedded into broader child health programs and systems; and second, the level of responsibility on the part of national government and reliance on external partners. There’s a wide spectrum along which countries might fall in each dimension.
- To be successful, integration of wasting services must be a health sector priority and the process must be led by the country government. Integration can be an extensive process. Government health sector leaders must own the process and value nutrition high on the UHC agenda in order to sustainably embed nutrition services within PHC. Support from development partners is needed along the way to support government goals.
- Integration is not an end in itself; rather, it can be an important means to help achieve program goals while moving toward universal health coverage. This means integration should be considered if it helps increase coverage and equity of services, reduce costs and increase efficiency of programs, and/or increase sustainability of the program and finances.
- The feasibility, risks and benefits of integration across all essential health and nutrition services must be considered. Integrating too quickly or where there is low capacity can overwhelm the system and end up reducing the quality of essential health and nutrition services. Integration must be assessed objectively for its overall impact on PHC as well as health and nutrition outcomes.
- Integration is not an all or nothing but a process: many forms of partial integration are possible across the health system. In many cases, the current state of integration is different across health system components and the guide covers each — leadership and governance, service delivery, health workforce, information systems, sustainable financing, and supply chain for ready-to-use therapeutic foods (RUTFs) — and also pays special attention to the emergency preparedness and resilience of wasting services.
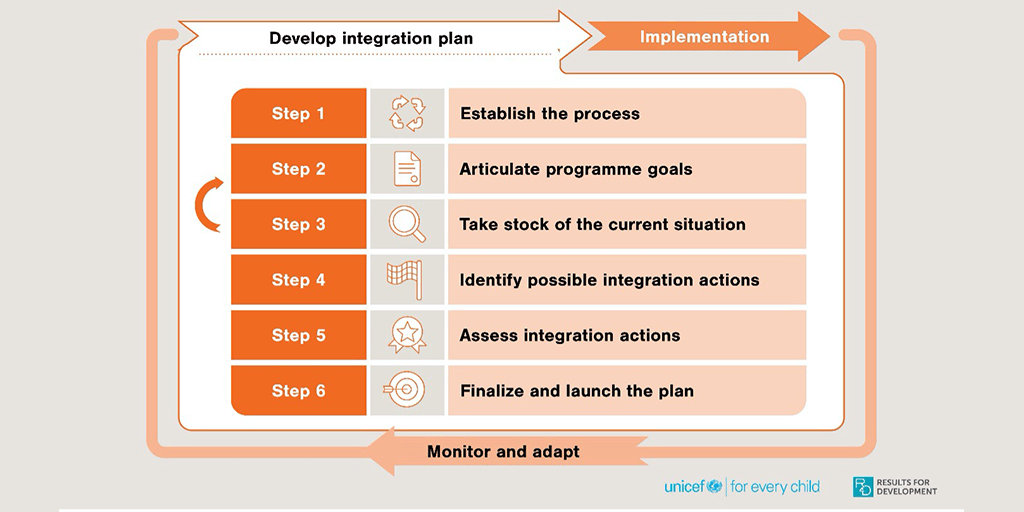
The guide offers a series of steps for countries to develop their integration plan (Figure above). While the focus is on integration of child wasting services, these principles and the approach to integration can be considered for a holistic package of PHC services that nutrition is part of.
We hope that the resources offered here help inspire national health leaders to take action toward achieving program goals for nutrition. We also hope it encourages all supporting partners — donors, technical assistance providers, and implementors — to follow the principles outlined above.
Photo © Clement Tardif/Feed the Future