Kenya’s Primary Health Care Bill: Another step forward but missing the link to other legislation
Kenya has implemented several strategies to make progress towards universal health coverage (UHC). The Kenya Primary Healthcare Strategic Framework 2019- 2024 emphasizes primary health care (PHC) as a vehicle for delivering UHC. The Community Health Policy 2020-2030 describes community health as an entry point into the health system, building on many decades of community health, which has been largely donor-funded, and lacks a legal framework for remuneration of community health workers. The Government recently proposed a new Primary Health Care Bill to strengthen PHC as part of a package of health legislation to further UHC. In this blog, authors review the bill and reflect on its strengths and weaknesses.
Another step in the right direction…
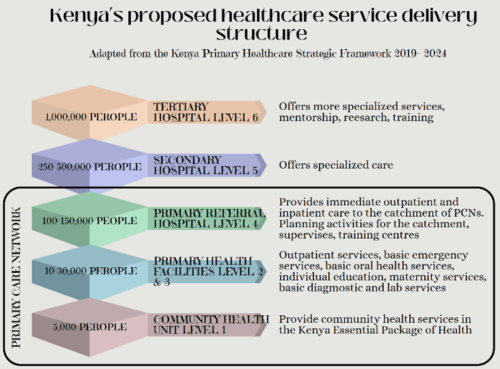
The bill articulates a vision for reorganizing PHC through primary care networks (PCN) and formalizing the delivery of community health through community health promoters organized in community health units. The primary care network is designed as a hub and spoke model, with multi-disciplinary teams at primary referral hospitals serving as hubs, supporting several spokes including dispensaries and health centers that are linked to community health units. The network aims to transform service delivery into a patient-centric model, improving integration of care, and facilitating referrals and gatekeeping between the hub and spokes.
In an unprecedented act, the bill recognizes community health promoters, defining their roles and recruitment through the county public service board, in essence inducting them into the ranks of county public servants and remunerating them accordingly. This is in keeping with the impetus to acknowledge the important role of community health workers and fairly remunerate them as in Brazil, Guinea and South Africa. Kenya’s national government is following through with this commitment, by equipping community health promoters with 100,000 kits in September 2023. The kits have basic health commodities and equipment for treating common ailments and measuring vitals.
The bill is missing links from other proposed legislation…
While the bill clearly lays out a new PHC structure, the financing aspects are less clear. This is especially problematic when one considers the other bills launched alongside it, including the Facilities Improvement Financing (FIF) Bill and the Social Health Insurance (SHI) Bill.
The FIF Bill provides health facilities with financial autonomy to manage revenue collected through user fees, insurance payments, and other sources. Currently, revenue from many dispensaries, health centers, and county hospitals is consolidated in the County Revenue Fund. Hence, facilities depend entirely on in-kind budgetary support from the county for health worker salaries, medicines, and consumables. This has denied facilities of resources and recourse to respond to local priorities as decision-making is centralized at the county level. The FIF Bill reverses this set-up, allowing facilities to retain revenue to pay for immediate operating costs (for example, buying out-of-stock medicines and covering maintenance, utilities or communications expenses as needed).
The FIF Bill says nothing about the Primary Health Care Bill, and the Primary Health Care Bill does not explain how primary care networks will receive and manage resources. Because of this, it is unclear if the individual facilities within the network will continue to budget and plan for their resources independently or as a group of facilities within one network. It also remains unclear how financial management of the network or individual facilities will be organized, or what financial accounting systems will be put in place within the network, and between the network and the county.
It would be reasonable to assume that a network design could benefit from economies of scale and enhance distribution of resources within the network. For example, if resources are managed within the network of facilities, they would need fewer accountants working across the network rather than having multiple accountants for each facility. They could also streamline administration by designating a unit within the network to work with the insurance agencies on preauthorization, claims submission and reconciliation. And it would be simpler for a payer to work with a few networks rather than many individual facilities. Financial management for a network raises other issues; for example, who takes responsibility for financial impropriety when it occurs. The bill may not include all these details, but it needs to at least lay out how these networks will broadly manage resources, while subsidiary regulations and policies describe these tasks in detail.
Just as the Primary Health Care Bill seems disconnected from the other bills the government has put forward, some of the other bills do not to link to the PHC Bill. The SHI Bill describes a Primary Health Care Fund through which public resources will be used to purchase services from health centers and dispensaries. It is noteworthy that the SHI Bill does not reference the Primary Care Network, even though many of the functions described in the bill such as benefits setting, tariff setting, accreditation, empanelment, contracting, and claims management will encounter these networks. There are unanswered questions, like does the Primary Health Care Fund purchase services from the Primary Care Network or from individual facilities, and will it cover community health services? The details on the Primary Health Care Fund are scanty and while subsidiary legislation is expected from the Ministry of Health, the links between the PHC Fund in the SHI Bill and the Primary Care Networks in the PHC Bill should be given greater consideration.
In summary, the PHC Bill enshrines commitments to improve the health and well-being of Kenyans through community health and Primary Care Networks. Studies have demonstrated the cost-effectiveness of interventions offered by community health units and well-functioning PHC facilities as compared to hospitals, which makes this a smart investment overall.
In addition to detailing how the Primary Care Networks and the community health units will be operationalized, more clarity is needed on how these will be financed and how they link with the financial arrangements envisioned by the FIF and SHI Bills. The three bills have been proposed at the same time, yet the lack of integration between them is a lost opportunity. Aligning these legislations now will go a long way in guiding the development of detailed implementation guidelines and their eventual roll out, improving the chances of success for these reforms to accelerate Kenya’s progress towards UHC.













