Pursuing public-private engagement options in mixed health systems
UHC Day 2019
[Editor’s note: This is the second post in a series of blogs sharing experiences from R4D’s work on mixed health systems. The authors of this series hope to encourage debate and the sharing of ideas on the topic of mixed health systems and public-private sector engagement for universal health coverage (UHC). This blog, in particular, explores how governments can support private providers’ integration into government plans. Catch up on the series, and read the first post, “3 principles for improving mixed health systems. The second post highlights the state of evidence around mixed health systems and what it means for the field.]
By R4D’s Adeel Ishtiaq, Cicely Thomas, Nathan Blanchet and PSI’s Rebecca Husband and Pierre Moon
In many countries, people rely on a variety of for-profit, not-for-profit and charitable small-scale private providers, maternity homes, and hospitals to access primary health care services, including maternal, newborn and child care and reproductive health and family planning. As health system stewards, governments can leverage existing resources available in the private sector to move closer to universal health coverage (UHC). They can also play an important role in helping to ensure the quality, comprehensiveness, and accessibility of services delivered by these private providers.
Some of the private providers providing services to women and children, in particular, are part of social franchise networks, such as those run-by or affiliated with Population Services International (PSI). Acting as an “intermediary,” PSI traditionally supports these providers in LMICs — often small-scale clinics — with training, supplies, and community engagement to provide high-quality services.
It has been proved that these social franchise networks can increase access to quality health care and provide a ready-built foundation for governments to expand access to health care. But there are sustainability challenges for maintaining the networks. The networks are often funded by donors, and, while in some countries, insurance exists to facilitate access, typically women and girls must pay out of pocket for key family planning services at the point of care.
Through a USAID-supported initiative, Support for International Family Planning and Health Organizations 2: Sustainable Networks (SIFPO2), R4D partners worked with PSI’s social franchise networks to help them become more financially sustainable while still maintaining access to quality services, including voluntary family planning.
Supporting the sustainability of private provider networks
Over 2015-2017, R4D worked with four PSI country teams to experiment with possibilities for connecting PSI provider networks with public sector funding. In Cambodia, Nigeria, Tanzania and Uganda, R4D joined the PSI teams and independent affiliates in conducting a landscaping of potential options for sustainability and provided varying levels of follow-up support to pursue the highest priority option in each setting. The work aimed to test how these provider networks, particularly those with established capacity, quality and links to public sector counterparts, might better position themselves to help contribute to national family planning and UHC goals.
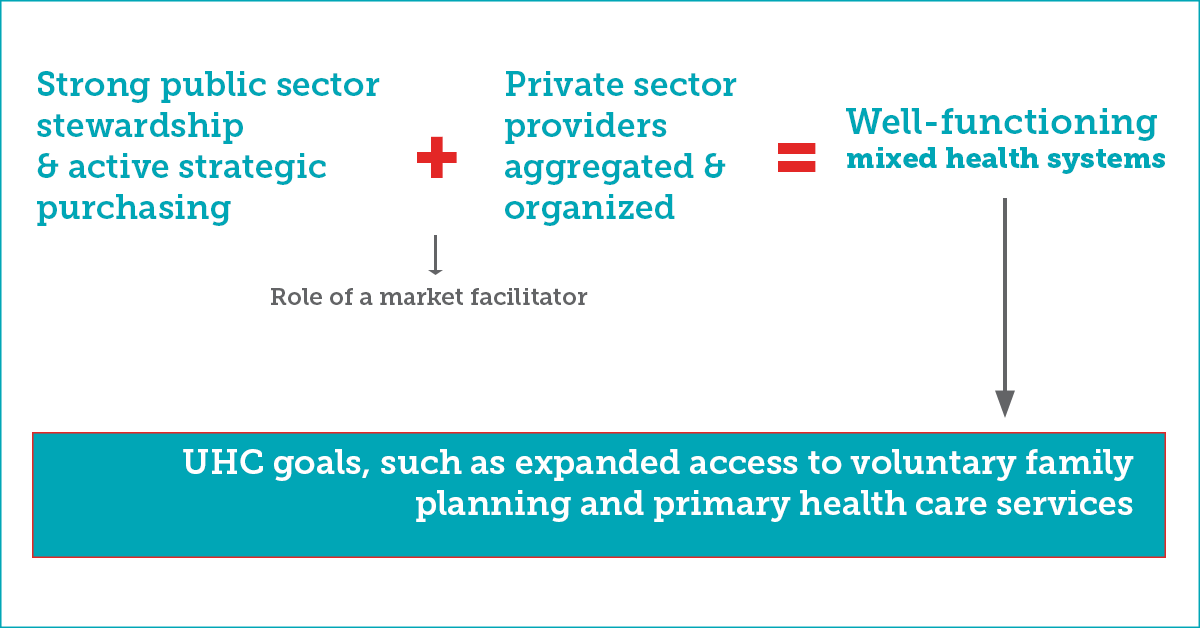
The work was based on the hypothesis that a ready provider “intermediary” can enhance the value governments see in engaging private providers by helping to design and implement contracts, among other roles. PSI teams and affiliates acted as the provider intermediary and, for the purposes of this limited initiative, PSI and R4D teams also acted as “market facilitators,” actively enabling dialogue, action planning and capacity building among public and private stakeholders. The figure below illustrates this general “facilitation-intermediation” approach:
What did we learn from supporting these private provider networks that is applicable to the broader discussion on supporting well-functioning mixed health systems?
We learned that while seismic shifts toward stronger mixed health systems in LMICs require a longer-term time frame, there were tangible wins from this work in terms of incrementally enhanced public-private engagement, which in this context related specifically to social franchise networks and engagement with government (more details on these learnings are available in Expanding Access to Voluntary Family Planning Services in Mixed Health Systems: Lessons from linking private health care networks to domestic financing). One of the greatest learnings from the work is the critical role governments must play as health system stewards to harness mixed health systems in service of public health goals. Specific learnings include:
1. Governments should focus on creating an enabling environment for engagement between the public and private sectors.
At the highest level, this requires an ideological orientation that is conducive to engagement among public and private actors. It also requires adequate capacity for public-private engagement in personnel and systems across the board, the presence of public sector champions with capacity and resources to drive specific initiatives, and mechanisms for both initial and routine communication between the public and private sectors.
In Uganda, SIFPO2 guided discussions between PACE/PSI Uganda and the Kampala Capital City Authority (KCCA), culminating in a concept note to “decongest” overcrowded public maternal health facilities by leveraging the resources of the private sector. This document then served as a blueprint for an eventual USAID/Uganda-funded partnership in 2018 between KCCA, PSI Uganda, and the University of Makerere School of Public Health to lead a three-year implementation science project, called the Maternal and Newborn Health (MaNe) Kampala Slum project, aimed at improving maternal and newborn outcomes in slum areas. However, stakeholders in Uganda note that public-private engagement like this seldom occurs because it can be hard for the government to be flexible and move quickly.
2. Governments should also help to set processes into motion to develop feasible approaches for leveraging private sector providers.
The facilitation-intermediation approach under SIFPO2 can be more broadly described as an example of “deliberative processes that raise awareness and identify solutions through analysis and structured dialogue among key stakeholders to enable public-private engagement.” We have written elsewhere about such deliberative processes in detail, noting principles that can make them more effective (covered in our previous post). To set such processes into motion, governments can proactively leverage the convening power and authority of trusted actors who enjoy the mandate of a broad array of health system stakeholders to promote greater public-private engagement. Provider associations, health care federations, and other suitable entities often already present in most LMIC contexts can be tapped for such a role, benefiting from government patronage and targeted assistance from its technical and funding partners.
For instance, in Lagos and Delta states in Nigeria, Society for Family Health has successfully worked to facilitate contracting mechanisms to manage and run public PHC centers — engaging the state ministries of Health and Wealth Creation as well as the state social health insurance scheme. In these examples, market facilitation worked best when the most authoritative stakeholders themselves endowed the facilitator with the ability to co-design a solution and align implementation.
3. Governments and their partners must identify and make essential reforms and investments to realize public-private engagement.
Some key prerequisites for successful public-private engagement include a clear sense among public sector officials of the gaps in the delivery and management of health services for which the private sector can be leveraged, a provider aggregator ready to act as an intermediary between public and private health sectors, and a public sector actually able to steward and eventually purchase from the private sector.
As a start, governments can begin to define and communicate public sector needs for private services as part of routine health planning and performance review processes — using standard templates to define target geographies, priority communities, and desired services and responsibilities. But to actually channel resources to private providers, governments must also reform rigid public financial management systems so as to give private providers adequate funding, the flexibility to plan its use, and clear performance standards.
***
Our work under SIFPO2 underscores that successful public-private engagement stems from proactive government stewardship of mixed health systems. It requires governments to play their role in transforming the environment in which engagement can take place, participate with enthusiasm in processes to join hands with the private sector around actionable ideas to address specific challenges, and invest resources and energy in certain essential first steps.