Amox DT, sustainable financing for health commodities and navigating donor-funding transitions: Lessons from Tanzania
It is rare for complex global challenges to be solved with a simple solution, but in the case of childhood pneumonia, a simple solution does in fact exist.
Amoxicillin dispersible tablets (Amox DT) is the preferred treatment for non-severe pneumonia in children under 5, as recommended by the World Health Organization (WHO). Amox DT is effective, lightweight, easy to transport without refrigeration and simple to dose. At about $0.50 USD per course of treatment, it is also relatively affordable — but maintaining consistent, long-term access requires reliable financing, especially when navigating the transition from donor support to domestic investment.
In line with its goal to reduce childhood mortality by 80% [1] by 2030, the Government of Tanzania (GoT), in collaboration with Results for Development (R4D) and other partners, has focused on addressing childhood pneumonia, the leading cause of under five deaths accounting for 15% [2] of all under-5 mortality cases.
R4D began working with the Government of Tanzania and other agencies in 2014 to improve Amox DT access, which was not widely available as a result of withdrawn donor funding and limited support for scaling up access. In the decade since that work started, R4D and partners have deployed a range of market shaping approaches to address barriers across financing, demand, supply and policy to support Tanzania as it transitioned to sustainable, domestic financing for Amox DT.
Amox DT financing
An examination of the market for Amox DT in Tanzania revealed several significant barriers. At the health sector level, the country faced financing challenges including limited domestic resources, delays in budget execution to the country’s national procurement agency — the Medical Stores Department (MSD) — and heavy reliance on donors, who were contributing approximately 48% [3] of the country’s health budget. These factors compromised the availability of life-saving health commodities and threatened the long-term resilience and sustainability of the country’s health system.
A deeper dive into financing for Amox DT uncovered no committed funding source for Amox DT. The imminent funding cliff created a high risk of nationwide stockouts. To address this urgent gap, R4D, with the support of its donor, GiveWell, mobilized catalytic, time-limited donor financing while simultaneously supporting the GoT to identify financing mechanisms to ensure long-term sustainability.
Using a co-designed approach, R4D conducted three strategic activities to advance sustainable domestic financing for Amox DT:
- Establishment of a co-financing agreement between MoH and R4D
- Exploration of sustainable financing mechanisms for Amox DT
- Development of a transition plan from donor funding to domestic funding
Establishment of a co-financing agreement between MoH and R4D
Establishment of a co-financing agreement between MoH and R4D
As catalytic donor financing for Amox DT was implemented, R4D established a five-year co-financing agreement with the GoT that required incremental, year-over-year increases in GoT co-financing, complemented by decreasing levels of donor funding for Amox DT (see Table 1 below). The goal of the co-financing agreement was to have the GoT fully and sustainably finance Amox DT needs by the end of 2022.
Table 1: Co-Financing Agreement between R4D and GoT
| Year | 2017 | 2018 | 2019 | 2020 | 2021 | 2022 |
| R4D/Donor Commitment | 100% | 90% | 70% | 50% | 40% | 0% |
| GoT Commitment | 0% | 10% | 30% | 50% | 60% | 100% |
Development of the co-financing agreement required extensive engagement with key government stakeholders including the MoH, MSD, PoRALG and the Ministry of Finance. After multiple discussions, the GoT endorsed the co-financing agreement and signed the agreement, which was then incorporated into the Memorandum of Understanding (MOU) between the GoT and R4D.
Initially, the GoT was on track to meet the funding targets set under the agreement, demonstrating strong desire towards sustainable financing of health commodities; however, the COVID-19 pandemic significantly disrupted progress placing immense pressure on domestic health budgets to effectively respond to the pandemic. Therefore, in 2020, the co-financing agreement was put on a temporary pause, with the GoT contributing 0% to the financing of Amox DT. During this period, R4D worked with the donor, who remained flexible and topped up to cover 100% of Amox DT procurement needs, ensuring continued availability and uninterrupted services (Figure 1).
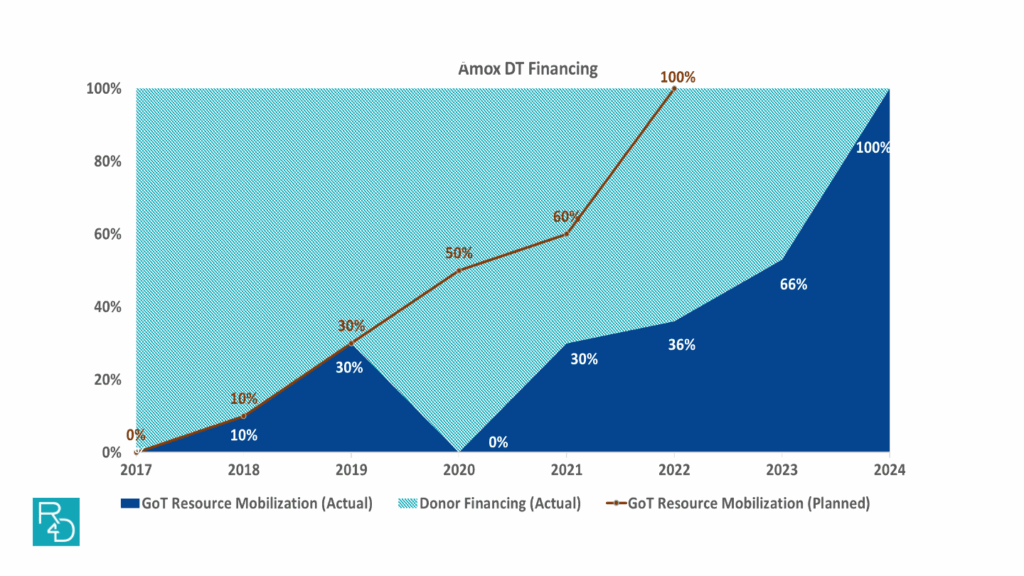
Figure 1: After the peak of COVID-19, the GoT refocused its efforts on the co-financing agreement, and incrementally achieved its goal of funding 100% of the country’s Amox DT needs through domestic resources by 2024. Efforts to achieve sustainable domestic financing for Amox DT spanned over seven years, extending beyond the originally planned five-year timeline.
As a result, Tanzania increased its domestic funding for Amox DT from $0 in 2017 to approximately $2.4 million by end of 2023, complemented by R4D donor-mobilized resources of approximately $3.8 million during the same period, equivalent to 18.8 million courses of treatment.
Through a systems-focused and collaborative approach to address key barriers and catalyze change, Amox DT availability significantly increased from 48% in 2017 to 93% in 2023.
Exploration of sustainable financing mechanisms for Amox DT
Exploration of sustainable financing mechanisms for Amox DT
In parallel with the co-financing mechanism, R4D provided comprehensive technical assistance to the GoT to explore options for sustainably financing Amox DT. We assessed several transition options, including maintaining Amox DT as a donor-funded product through continued government-led resource mobilization; funding the treatment through central government allocations; or a transition to purchasing Amox DT from MSD by health facilities through health facility budgets.
After careful review, utilizing health facility budgets was determined to be the most sustainable approach, given the following considerations:
- Avoiding reliance on donor funding and promoting sustainability
- Feasibility of health facilities to purchase from their own budgets, given that Amox DT is a low-cost medicine ($0.50 per course of treatment)
- Strong incentives to prioritize purchase (Amox DT is a tracer item, and facilities are required to maintain stock)
- High demand for Amox DT at the facility level, which supports the sustainability of this approach
Development of transition plan from donor funding to domestic funding
Development of transition plan from donor funding to domestic funding
To ensure a smooth transition from donor funding to domestic funding, R4D and the GoT developed a transition plan with a focus on ensuring timely and clear communication with key stakeholders (Figure 2).
Key steps included:
- Sharing an internal memo to notify the MoH about the end of donor funding for Amox DT to initiate early transition planning
- Holding early discussions about the transition to domestic financing with key stakeholders such as health facilities and MSD to ensure awareness and allow adequate time for planning for their respective business processes (i.e. ordering, procurement, etc.)
- Developing a communication strategy with the government partners, identifying what communication needed to go out, to whom and by when
- Implementing the communications strategy and disseminating official notices of transition to MSD and health facilities
- Ensuring procurement of the first planned, fully government-funded consignment
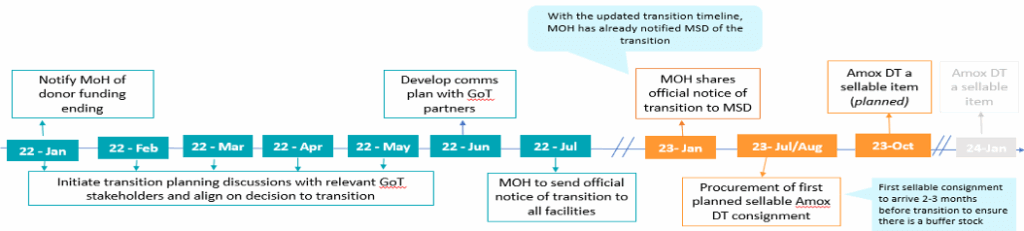
Figure 2: Transition plan
What is the status of Amox DT financing and availability in Tanzania today?
Today, Amox DT remains fully funded through domestic resources, leveraging both health facility budgets and central government funds. However, while the first six months of the transition were smooth with high availability of Amox DT maintained, several challenges have emerged in subsequent months. Challenges observed include delays in procurement and clearance at the port of entry, delays in fund disbursement to the suppliers, delays of delivery by suppliers among others, which have led to a decline in availability from an average of 93% in 2023 to 80% in 2024.

Key lessons learned
Key lessons learned through the implementation of this program include:
- The co-financing agreement between R4D and the GoT and the transition plan played a critical role in facilitating gradual domestic resource mobilization while ensuring smooth transition and minimum impact on product availability levels.
- Flexibility and adaptability are essential. The donor’s ability to adjust during COVID-19 disruptions allowed the program to stay on track toward achieving the goal of sustainability through domestic resources.
- Strategic use of catalytic donor funding played a crucial role in bridging critical financing gaps for Amox DT, and it ensured continued access to this life-saving product while providing opportunity for the government to identify sustainable funding mechanisms. This approach highlights an effective way to align donor support in filling temporary gaps without duplicating efforts while supporting sustainability through local ownership.
- To ensure sustainability, solutions must be embedded within government structures rather than creating parallel systems. This works best when government leaders and other change agents are in the driver’s seat, as they are the ones that are most aware of how to integrate new solutions into existing systems. For example, financing of Amox DT was embedded into direct health facility financing mechanisms, leveraging health facility budgets as a sustainable financing source for Amox DT.
- The transition plan ensured timely notification to all key stakeholders including MSD and health facilities, allowing sufficient time to align and prepare which enhanced a smooth transition.
- Commodity financing, while significant, is one element of a healthy market and does not guarantee product access and availability. As seen with the Amox DT example, despite having sustainable financing sources in place, availability is still a challenge and other key market and supply chain functions must also be an area of focus (i.e. procurement, supply planning, manufacturer selection, etc.).
- The Amox DT approach offers a replicable model for other essential medicines. Its successful transition from donor reliance to sustainable domestic financing demonstrates that embedding solutions within government systems, leveraging catalytic funding to bridge gaps, co-designing transition plans with national stakeholders, and maintaining clear communication are transferable strategies. When adapted to the specific context of other products, these elements can support countries in reducing donor dependency and promoting long-term sustainability through domestic resources.
- Sustainable change takes time. The Amox DT experience highlights the importance of prioritizing sustainability at the outset, with all activities designed to support this goal – a critical factor in the program’s success. Over seven years, Tanzania fully transitioned Amox DT procurement to government funded, offering a model for reducing donor dependency through strategic planning, government leadership, and adaptive execution.
The journey toward sustainable financing for Amox DT in Tanzania demonstrates how strategic planning, adaptive implementation and strong government leadership can drive sustainable transitions from donor reliance to domestic resource mobilization. Key lessons such as embedding solutions into government systems, leveraging catalytic funding to bridge gaps, and maintaining flexibility offer a replicable model for other essential medicines. Ultimately, long-term sustainability requires patience, partnership, and an unwavering focus on building capacity within existing structures.
References
- Government of Tanzania, Ministry of Health and Social Welfare, “Women and Children First: Countdown to ending preventable maternal, newborn and child deaths in Tanzania” (2015).
- UNICEF, World Pneumonia Day graphics (2015)
- Tanzania Health financing profile (2016)













