COVID-19’s Impact on Strategic Health Purchasing: Lessons from Ukraine
Collectivity Series: 5 of 5
[Editor’s Note: This is the second post in a blog series by a group focused on strategic purchasing, working through Collectivity — a collaborative learning platform for global, regional and country experts. This series features insights from six country teams that explored how governments have adjusted their health purchasing arrangements to support the COVID-19 health response, as part of a project co-facilitated by R4D, the Strategic Purchasing Africa Resource Center and the World Health Organization. Jointly, these country teams are seeking to draw lessons for the future, and share reflections on whether these adjustments contribute to making purchasing more strategic. In this post, the Collectivity’s Ukraine team shares takeaways from the adjustments the government made in purchasing arrangements for health services (and their linkages with the health sector reform in Ukraine).]
The Ukrainian health system is an illuminating example of a health system attempting to utilize a health shock to build health system resilience as well as build on its health system reform potential to dynamically address challenges. COVID-19 struck Ukraine in early 2020 while the health financing and provider payment reform was still in its incipient stages. Rather than derailing the reform process, Ukrainian government utilized the crisis to successfully accelerate its progress in the flagship health reforms, including the setup of the Program of Medical Guarantees (PMG), to advance access to universal healthcare. This was achieved by the initiation of new policies that were aligned with PMG goals, reinforced by key innovations and prioritized health funding, amounting to USD 1.7 billion of COVID-19 allocations to health. Significantly, the government offered coverage for all COVID-19 related care and diagnostics free of charge; embraced digital technology for evidence-based decision-making in service provision and monitoring; deployed financial incentives to address health system inefficiencies; incentivized attraction of a new cadre of medical personnel; and flexibly expanded and financed provider network as a quick pandemic response.
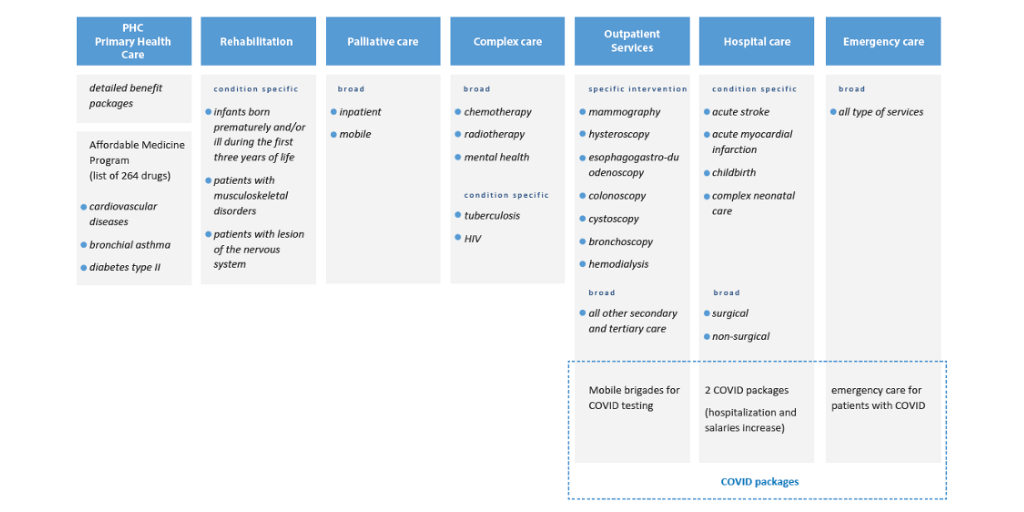
Ukraine’s nascent health reforms aimed at delivering universal, timely access to integrated care. The Law on Financial Guarantees for Health Care Services of 2017 defined a guaranteed benefit package for all Ukrainians through PMG and established the National Health Services of Ukraine (NHSU) as the strategic purchasing agency for this program, granting considerable flexibility. This flexibility and political support also allowed for quick adjustments in purchasing arrangements to changing COVID-19 health care needs during the pandemic. The NHSU is entitled to purchase PMG services through packages defined on annual basis with regular adjustments to accommodate evolving needs (Figure 1).
Figure 1: Services packages purchased under the PMG in 2020
Source: Health Financing Reform in Ukraine: Progress and Future Directions. 2021. WB and WHO joint report.
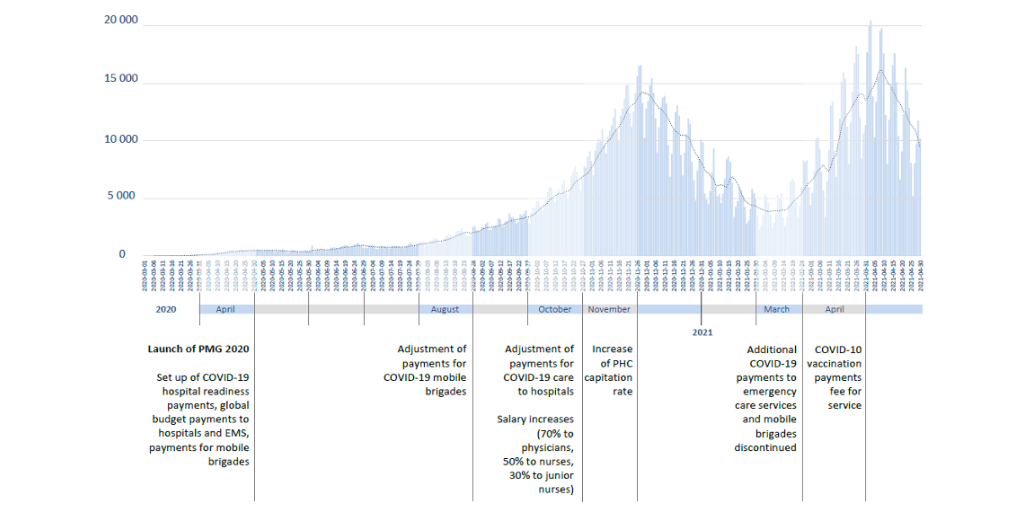
The ongoing reforms to a certain extent accelerated by the pandemic enabled Ukraine to transition from historically line-item budgeting towards modifying purchasing arrangements for channelling resources to selective health providers conditional on confirmed provider capacity using new payment mechanisms (capitation, global budgets, fees for service, per-case payment etc). Ukraine was not only able of using the new payment mechanisms to introduce new COVID-19 services through the network of existing providers, which have been able to reprofile their capacities to the new challenges of the health system, its new purchasing arrangements were flexibly amended to react to the surges of COCID-19 cases and service delivery patterns, as presented in figure 2.
Figure 2: Mapping of the Health Financing Decision and COVID-19 Waves in Ukraine
It is an opportune time to reflect on whether Ukraine’s pandemic response affected the health system reforms and how the adjustments made in purchasing arrangements helped these health system reforms to progress.
As part of the collaborative learning Collectivity project on Strategic Purchasing and COVID-19 this blog assesses the adjustments made in purchasing arrangements and their linkages with the health sector reform in Ukraine. Below, we share three key takeaways from our research.
1. Criticality of the existing foundation as a pre-requisite to the COVID-19 response
The ambitious reforms spurred a series of transformative structural changes that provided an advantage for quick COVID-19 health sector response with regards to purchasing of services, information, and human resources management. NHSU as the single purchaser invested in building an integrated health system by reorganizing healthcare delivery with primary care designed to serve the gatekeeping function. With coverage of over 70% population, the PHC provided the cardinal network for collection of COVID-19 test samples, outpatient treatment and vaccination delivery. Select facilities upon the fulfillment of service delivery requirements were contracted and offered readiness packages designed to provide inpatient COVID-19 care.
In parallel, NHSU starting with simple excel-based data collection in 2020, worked to strengthen the national e-health information system to build the architecture supporting the contract management and payment to contracted COVID-19 health providers while minimizing potential fraud through data e-verification. Furthermore, the e-health system also facilitated innovative service delivery such as teleconsultation by maintaining electronic patient health records, e-referrals, e-prescriptions and creating the potential for better coordination of patient pathways following COVID-19 protocols whilst addressing the demand for essential health services.
2. Existing governance arrangements helped flexibly refine COVID-19 purchasing decisions
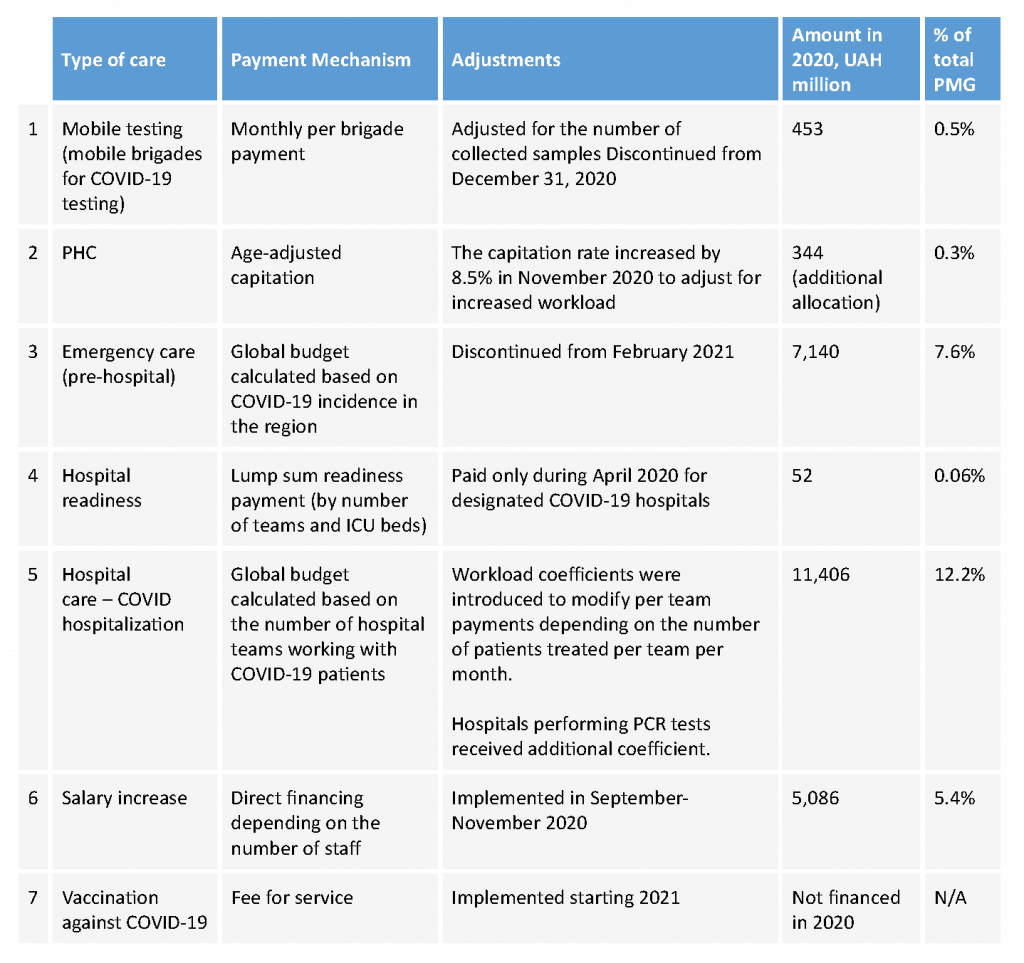
Adjustments made to the existing purchasing arrangements of the network of healthcare providers were instrumental in the implementation of the COVID-19 response in Ukraine. The existing benefit package and purchasing arrangements were quickly upgraded to include new services packages for treatment, testing by mobile brigades, COVID-related emergency care, vaccination. It also included financial incentives to medical personnel to adjust for COVID-19 burdens. Table 1 presents the variety of purchasing mechanisms and their adjustment that were introduced in 2020.
The revised benefit packages covered the PHC cost of setting up mobile teams for sample collection (eventually discontinued). The capitation payments to PHC providers were adjusted by an increase of 8.5% to reflect the growing COVID-19 workload, but this was just a minor adjustment that increased PHC share in the PMG by 0.3%, amounting to 19% of PMG Budget. The pay for COVID-19 vaccinations was later introduced in 2021 to cover expenditures and incentivize providers to effectively rollout COVID-19 vaccination.
Transitioning from the historical input-based budgeting, specialized care purchasing, including COVID-19 packages, used a mix of purchasing arrangements, predominantly global budgets, amounted to a massive 81% of PMG Budget, of which 20.4% was allocated to finance COVID-19 care. This allowed providers to cover losses from the hospital payment reform process, provided financial bonuses to COVID-19 warriors and compensated hospitals for COVID-19 additional expenses. The expansion of the financial envelope disproportionately directed funds towards specialized care, suggesting losing potential efficiency gains from parallel adequate efficient investment in primary care.
Table 1: COVID-19 purchasing arrangement and adjustments implemented in Ukraine
3. Overarching Challenges in the Health System and Health FinancingThe well-intentioned new provider payment mechanisms that have been introduced simultaneously with the COVID-19 pandemic crisis were mostly output-focussed and hoped to achieve higher efficiency through greater spending flexibility, output-based contracts, and provider autonomy. However, the pandemic inadvertently created a perverse incentive for local governments and hospitals to demand an expansion of COVID-19 providers as means of securing additional funding and providing COVID-19 care at the nearest care facility. Consequentially, there was a spurt in additionally designated hospitals with significantly increased budgets and compromised quality of care. Despite adjustments to purchasing arrangements to reflect outcomes (number of patients treated each month) instead of capacity (number of doctors), periods of low incidence of COVID-19 cases with low workload for facilities resulted in inefficient health spending. Hence, there is a considerable scope for improving quality and intensity of service provision by introducing complimentary monitoring framework to benchmark performance across facilities with the potential result in improved accountability.
Undoubtedly, there are more efforts ahead as Ukraine continues its health system transformation. The pandemic has delayed the intended transition of purchasing arrangements towards a more standardized and cost-effective hospital financing using case-based payments based on diagnosis-related groups, instead using global budgets and fee-for-service payment method for specialized care by 2020. The hurried process of contracting providers, deficiencies of provider licensing and opaqueness designing PMG benefit packages that do not clarify the full scope of all services covered by PMG creates another overarching challenge. The political turbulence including frequent change of leadership in the Ministry of Health and NHSU during the critical months of the pandemic also exacerbated trust in public institutions. Overall, low trust to public services is also associated with COVID-19 vaccine hesitancy, and low adherence to social norms.
Finally, recognizing NHSU as a young central purchasing agency while it was thrown in the deep end with the additional demand of pandemic preparedness and response is imperative. The smooth adaptation of budget planning and COVID-19 financing was dented by serious implementation and operational challenges due to NHSU’s limited experience with strategic purchasing necessitating the demand to continuously evolve in a dynamic and challenging environment. Providers also had limited to no experience of working under the new payment arrangements, which created accountability and governance challenges, such as continuation of informal payments, or accumulation of funds on deposit accounts instead of financing services. Investing in strengthening of institutional and organizational capacity to make purchasing more strategic implies using strong information system to ensure effective performance of contracted providers, monitor and evaluate UHC progress, facilitate stakeholder consultations and manage coalitions with government is pertinent.
The insights provided in this series are part of a larger research effort — led by Collectivity country teams — on the strategic purchasing reforms countries developed during the COVID-19 pandemic. Their collective research will culminate in a series of published journal articles. Click here to learn more on the Collectivity Group on Strategic Purchasing, which aims to contribute to the global knowledge base on strategic purchasing and strengthen the ecosystems that support countries to advance health financing and health system reforms.
Catch up on the Collectivity Blog Series