Empowering champions through learning: Reducing childhood pneumonia in Tanzania
No child should die from a preventable and easily treatable disease. Despite significant global progress over the last decade in improving child mortality rates, pneumonia remains the leading infectious killer of children under 5 years old. In 2019 alone, pneumonia killed more than 740,000 children under 5 worldwide — and in Tanzania, pneumonia accounted for 15% of child deaths, stubbornly remaining the leading cause of child mortality.
It’s not often that the most vexing global problems can be solved with a simple solution, but in the case of childhood pneumonia, a simple solution does exist. Amoxicillin dispersible tablets (amox DT) is the preferred treatment for non-severe pneumonia in children under 5, as recommended by the World Health Organization (WHO). Amox DT is effective, lightweight, easy to transport without refrigeration, and simple to accurately dose. It’s also relatively affordable at about $0.50 USD per course of treatment.
With its goal of reducing child mortality by 80% by 2030, the Tanzanian government has been championing the fight against pneumonia and has prioritized efforts to address childhood pneumonia, but scaling up the use of amox DT across the country has proven challenging.
Since 2015, Results for Development’s Market Shaping Practice (MSP) has partnered with the government of Tanzania to implement a holistic market shaping program to ensure that amox DT is consistently accessible to the children who need it. R4D and the government have collaborated to ensure the country has the funding it needs to buy and maintain a steady treatment supply and to address underlying barriers affecting whether amox DT is available at health facilities and accurately prescribed.
To read more about the impact of this work, visit this page.
Supporting impact through learning
Together, R4D’s Market Shaping Practice and the government of Tanzania achieved remarkable progress in improving the funding, procurement and supply of amox DT in Tanzania, making progress toward averting preventable deaths from childhood pneumonia. Funding and supply alone, however, are not enough to save children’s lives. To do this, amox DT must be available at the right place and right time, and it must be prescribed appropriately to the children who need it. Data and evidence are required to know whether this is happening successfully — or not — and to understand what might need to improve and how those improvements can be made.
To achieve and measure its impact, MSP partnered with R4D’s Evaluation and Adaptive Learning (EAL) practice to bolster the program with ongoing data and evidence use. Beyond measuring outputs and outcomes, the EAL approach helps partners ask targeted questions about their program activities, get answers at the right time, use this information to facilitate continuous program improvements and strengthen local capacity for continued monitoring and evaluation success. Throughout the project, EAL team members worked closely with MSP and the Tanzanian government to identify key learning questions and develop ongoing monitoring and learning activities to address them.
Identifying the learning questions
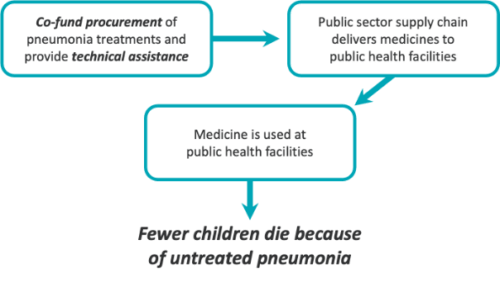
The team first began identifying learning questions with the understanding that the success of amox DT market shaping efforts relies on the functioning of the underlying system. A simplified version of that system is shown below in Figure 1. In order for technical assistance and co-funding of amox DT procurement to be effective, and in order to prevent child deaths from untreated pneumonia, the medicine must be effectively delivered to health facilities and used by providers.
To understand whether this was happening within Tanzania’s health system — and how — the team worked with the government to develop a more detailed map of the process that takes place within the system. The more nuanced understanding of the system drew on multiple data sources and methods, including administrative data, stock monitoring data and other formative research. As the team learned more about the system and all the steps in the process from procurement to prescription of amox DT, this map became more and more complex, as seen in Figure 2 below, which is a more detailed version of Figure 1 above.
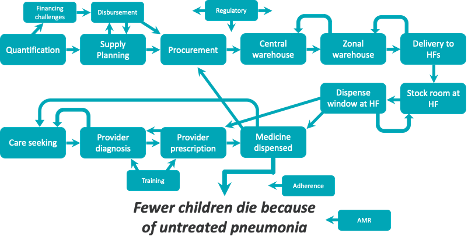
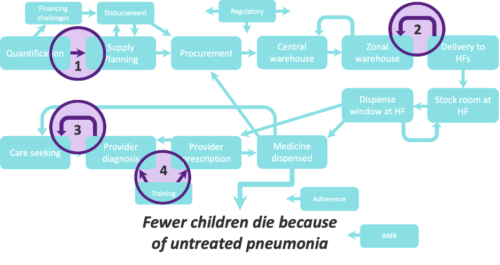
As the team’s understanding of the system and its complexity grew more sophisticated, we were able to work with the Tanzanian government and identify potential bottlenecks, areas of uncertainty and critical questions where additional evidence and testing could be used to inform and improve the work of the program, and designed research and learning activities to address them:
- How can quantification and procurement be improved to avoid stockouts and oversupply of amox DT?
- Is amox DT reaching health facilities where and when it is needed?
- Is amox DT reaching the children who need it?
- How can diagnosis and treatment for childhood pneumonia be improved?
How can quantification and procurement be improved to avoid stockouts and oversupply of amox DT?
Making sure facilities can get sufficient supplies of medicine when they need them starts with first buying enough supplies to stock the national medical store. The national medical store figures out how much stock to have on hand based on high-quality quantification and supply planning. The government believes high quality quantification is based on aggregating data from across the entire country on what individual health facilities say they need (i.e. the bottom-up quantification approach).
However, in its current state, the system is not set up to pull this kind of data in an accurate, rigorous, or clear way.
The systems need to evolve so that facilities can easily calculate and then report on what they need. R4D worked with the government to review their existing systems and create a plan of action for revising the current quantification approaches and for supporting health facilities to participate in this new approach. This resulted in the development of the bottom-up quantification roadmap, which over time and once implemented, should lead to more accurate quantification.
Is amox DT reaching health facilities where and when it is needed?
Improvements to the quantification and procurement of amox DT supply at the national level should then cascade through the health system and lead to greater availability of amox DT where it is needed most: on the shelves of health facilities.
R4D conducted a nationally representative health facility survey across 11 rounds of data collection. This allowed the team to track the fluctuations in availability and stocking overtime. It confirmed that amox DT levels increased to much higher levels and consistently stayed at those much higher levels.
The independently collected data also provided a way to triangulate the availability trends with existing government data bases. Whereas at the beginning of the program, many stakeholders worried about the data quality in these government data bases, toward the end, many reforms (not tied to R4D) had led to better data tracking.
The triangulation exercise confirmed that availability between the government data system and the independent data collection process were similar, instilling confidence that the government data systems were an accurate data source to monitor commodity availability in the long run.
Is amox DT reaching the children who need it?
While improving the supply of amox DT and ensuring its availability at health facilities are critical steps, amox DT will not ultimately help save children’s lives unless childhood pneumonia is accurately diagnosed and the treatment is appropriately prescribed. If pneumonia is under-diagnosed, amox DT may not reach children who desperately need it. On the other hand, if pneumonia is over-diagnosed, amox DT may be overprescribed, leading to concerns about the development of antibiotic-resistant disease.
To better understand diagnosis and prescription behavior among health providers in Tanzania, the team designed and implemented an innovative clinical study in 2017. Conducted in 83 public health facilities in the Pwani, Dodoma and Tabora regions, the study utilized a novel method of estimating under- and over-diagnosis of pneumonia in children under 5 by comparing directly observed public provider diagnoses to the results of diagnoses made by trained clinicians using lung ultrasound machines.
During the study, the team observed 93 providers conducting exams on patients aged 2 months–5 years who presented respiratory symptoms or were given a respiratory diagnosis by the provider. Overall, only 17.6% of cases confirmed as pneumonia via lung ultrasound examinations were also diagnosed as pneumonia by providers, suggesting that a significant number of pneumonia cases for which care is sought in the public sector go undiagnosed. Further, the team discovered key gaps in the diagnostic process that could be contributing to underdiagnosis. For example, providers conducted a clinical examination on only 33% of children and counted the breaths per minute (the most important diagnostic step) on only 13% of children.
How can diagnosis and treatment for childhood pneumonia be improved?
As results from the diagnosis and prescription study showed, providers often struggle to reach a correct diagnosis. The Tanzanian government was heavily committed to better understanding what factors may help improve diagnosis.
Rather than try something untested at a large scale, the team aligned with the Tanzanian government for lean, small-scale testing of several possible interventions that could improve diagnosis and prescription behavior.
The team leveraged the know-can-do framework to design possible interventions for the first round of lean testing:
- The first set of interventions focused on ensuring that providers had the knowledge (know) so that they were capable (can) of appropriate diagnosis. The interventions included text message reminders, visual aids and clinical mentoring. Mentoring was the most promising and visual aids were the least promising because of the quick drop off in engagement with the material, which would lessen the knowledge gains over time. Two-way messaging (i.e., a more interactive text message thread with a provider) provided more engagement. Lessons from mentoring and two-way messaging highlighted the need for future focus on relationship building and engagement.
- In a second round of lean testing, the team workshopped ideas with a broad range of government and non-government stakeholders, sharing the lessons from the first round, and focusing on identifying priority interventions that will help providers actually perform (do) the steps.
During the workshop, stakeholders identified that while clinicians have the knowledge and are capable of conducting the right steps to reach appropriate pneumonia diagnosis, they do not perform these tasks due to various barriers, including overwhelming lines to seek care, resulting in lack of adequate time to perform the appropriate diagnosis steps.
As a result of this conclusion, the intervention that was tested was to increase the involvement of the triage nurse in the health facility by having them conduct the pneumonia diagnosis steps on children presenting with respiratory symptoms and flagging the clinician when pneumonia diagnosis was being considered, with the aim of having clinicians repeat the steps and confirm the pneumonia diagnosis. Nine triage nurses received a refresher training on the Integrated Management of Childhood Illness (IMCI) steps for pneumonia diagnosis and thereafter, the intervention of the triage nurse conducting the diagnosis steps was implemented in nine health facilities.
From observation and data collected, some of the key learnings from the lean testing included that triage nurses can conduct pneumonia diagnosis steps, and more steps are done when both the clinician and triage nurse are responsible for conducting IMCI, leading to a greater chance of accurate diagnosis. However, significant quality of care gaps remains across both nurses and clinicians and performance rapidly declined after the training, indicating that both provider types need more support to improve overall quality of care.
Further research in this area could also unpack findings around the impact of the facility context on provider performance, due to how nurses and clinicians within the same facilities appeared to perform as teams.
The childhood pneumonia program in Tanzania provides some critical lessons for those that are championing the fight against pneumonia globally:
- Partnership, leadership and ownership from country governments is critical to success. The Tanzanian government embarked on a journey with R4D and remain committed in its fight against pneumonia, leading to sustainable ownership of financing and procurement of amoxicillin dispersible tablets over time.
- Market shaping at the country level, with a focus on working with local change agents and designing for sustainability, provides a holistic framework and approach to scaling up access to life saving commodities.
- Embedding an evaluation and adaptive learning approach within programs can provide access to rich data in a relatively short period of time, allowing for data-driven decisions to be made for program design and policy change














