Toolkit Home / What is the Strategic Health Purchasing Progress Tracking Framework?
Overview of Strategic Purchasing
Health purchasing refers to the transfer of pooled funds to health providers in exchange for delivering covered services. Purchasing is one of the functions of health financing systems – revenue raising, pooling and purchasing. Purchasers can be either passive or strategic in how they transfer these funds. Passive purchasing implies following a predetermined budget or simply paying bills when presented without considering how to be more efficient in health spending. Strategic purchasing is deliberately directing health funds to priority populations, interventions, and services, and actively creating incentives so funds are used by providers equitably and in alignment with a population’s health needs.
“Purchasing” is the transfer of pooled funds to health providers. It is considered strategic when information is used to link resources to population health needs.
Many countries have made political commitments to Universal Health Coverage (UHC), but as of 2021 about 11% of the world’s population lived in countries that spent less than US$50 on health per person per year.1 Strategic purchasing of high-priority health care services can be a powerful means for advancing UHC goals. Purchasing health care services more strategically means using evidence and information about population health needs and health provider performance to make decisions about which health services should have priority for public funding, from which providers those services should be accessible, and how and how much providers should be paid to deliver these services. Strategic health purchasing is generally accepted in the global health community as a critical lever to facilitate progress toward UHC within fiscal constraints.2Terminology
About the Framework
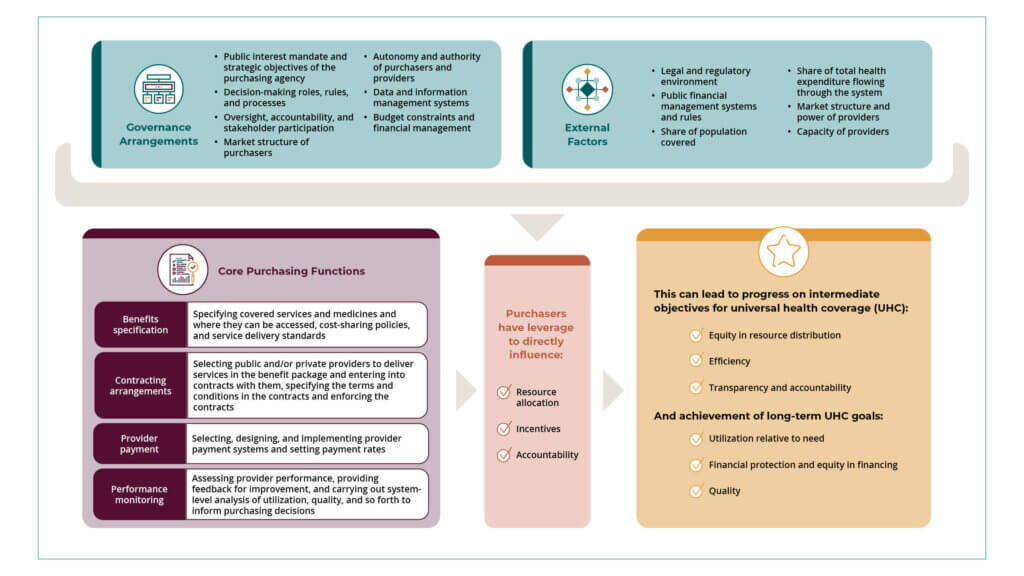
The Strategic Health Purchasing Progress Tracking Framework is a practical framework and approach to understanding purchasing of health services. The Framework builds upon other strategic health purchasing resources3,4,5,6 and combines the conceptual framing of strategic purchasing with practical guidance on describing and assessing purchasing functions systematically and in sufficient detail to inform policy decisions. The Framework was co-created by a group of health financing researchers and academics through SPARC and focuses on the core purchasing functions of benefits specification, contracting arrangements, provider payment and performance monitoring. It incorporates factors that can either strengthen or weaken the power of purchasers to directly influence resource allocation and provider behavior.
In many countries, there are multiple health financing schemes or purchasing agencies that channel resources to providers for delivery of health services. These may include the government budget channeled through Ministry of Finance or Ministry of Health, National or Social Health Insurance Agency, vertical health programs (for HIV&AIDS, tuberculosis, malaria, immunization, family planning), private health insurance or community-based health insurance. Providers may include different types of health facilities – primary healthcare facilities such as dispensaries, health centers, secondary or district hospitals and tertiary hospitals. Providers may have different ownership including government-owned/public, private, faith-based or nongovernment organizations. Rather than focus on any one individual scheme, we suggest applying the Framework in a way that describes how the purchasing functions are carried out across the most important health financing schemes in the country. When the Framework is applied in this way, it can provide a more complete picture of purchasing across health financing arrangements to identify areas of progress that can be built on and areas of fragmentation or overlap that need to be addressed.
The terms “purchaser” and “purchasing agency” refer to any entity responsible for purchasing services on behalf of a population. Examples include the Ministry of Health (MOH) in a supply-side budget system, a designated department within the MOH, or a national or subnational health insurance agency.
Terminology
The image below illustrates the Strategic Health Purchasing Progress Tracking Framework:
Application of the Framework has shown the value of mapping purchasing functions across multiple health financing schemes to identify where strategic purchasing progress is more advanced and where it may be lagging. It has helped countries identify challenges—such as fragmentation and duplication of purchasing functions across health financing schemes—and prioritize policy actions.
For more information on the Framework, review this article by Cashin and Gatome-Munyua.
Learn from experts on the Strategic Health Purchasing landscape in Ghana and Burkina Faso:
Why use the Strategic Health Purchasing Progress Tracking Framework?
The Framework can support countries to:
- Take practical steps to improve purchasing incrementally, in a way that can be scaled systemwide and is not limited to marginal innovations or a single purchaser.
- Identify opportunities for improvement at the health system level across different purchasers through changes in national policies, health system institutions, and governance.
- Identify opportunities for improvement at the purchasing agency level through changes in provider payments, policies and governance, and operations.
Learn about the relevance of the Framework from experts who have applied it in their countries:
How application of the Framework has informed health purchasing improvements
Spotlight on Rwanda
Rwanda is well known for its high insurance coverage through the Community-Based Health Insurance scheme, which covers about 93% of the insured population. In 2017 Rwanda began development of a Health Financing Strategic Plan (HFSP) for the first time. As part of the development of the strategy, there was an analysis of health financing functions, including purchasing. The strategy highlighted some of the gaps in purchasing but not enough to know how to address them.
In 2019, University of Rwanda School of Public Health was one of eleven partners that co-developed the Strategic Health Purchasing Progress Tracking Framework. Applying the Framework in Rwanda was motivated by the interest to implement the HFSP. Through a country-led partnership between the University of Rwanda School of Public Health, the Ministry of Health and the Rwanda Social Security Board (RSSB), the three stakeholders led by University of Rwanda School of Public Health applied the Framework including the data collection, analysis and dissemination of findings.
The assessment included the government budget, Community-Based Health Insurance and the RSSB medical scheme. The assessment7 found that Rwanda has made progress in many areas of strategic health purchasing, such as consolidating purchasing functions under the RSSB, having a purchaser-provider split, contracting providers and monitoring of provider performance and quality of care. This has led to better access to care, more financial protection for citizens, and overall better health outcomes.
However, there are some areas for further improvement revealed during the application of the Framework such as overlaps and duplication of functions across health financing schemes, as well as financial sustainability challenges in the Community-Based Health Insurance scheme due to open-ended fee-for service payment.
Everyone was very surprised with the level of detail of the findings and how well they mirrored current purchasing practice. Policymakers were eager to participate in efforts to respond and address the findings. Stella Matutina Umuhoza MPH, MSc
As a result of applying the Framework as a collaborative learning process, Rwanda policymakers began working on several incremental improvements:
- The process to adjust the Health Benefit Package was not evidence-based in the past, therefore a committee was put in place to develop criteria for inclusion of services in the benefit package, and the University of Rwanda School of Public Health led the technical analysis to determine how to cover care for 67 cancers.
- A technical working group was established to oversee the design of a capitation model for primary healthcare services, which was adapted to the Rwandan context.
- Policymakers are also revising the relevant M&E and policy frameworks for provider payment to ensure the process of review of provider payment is free of any real or perceived conflicts of interest.
Rwanda continues its journey to improve purchasing to improve efficiency and resource allocation and ultimately to make progress on coverage goals and financial protection of its citizens.
For a full list of citations, see the pdf version of the toolkit.