COVID-19’s Impact on Strategic Health Purchasing: Lessons from Armenia and Romania
Collectivity Series: 2 of 5
[Editor’s Note: This is the second post in a blog series by a group focused on strategic purchasing, working through Collectivity — a collaborative learning platform for global, regional and country experts. This series features insights from six country teams that explored how governments have adjusted their health purchasing arrangements to support the COVID-19 health response, as part of a project co-facilitated by R4D, the Strategic Purchasing Africa Resource Center and the World Health Organization. Jointly, these country teams are seeking to draw lessons for the future, and share reflections on whether these adjustments contribute to making purchasing more strategic. In this post, the Collectivity’s Armenia and Romania team shares three lessons on the role of strategic purchasing amid a pandemic, based on how both countries created fiscal space and adapted their purchasing arrangements to respond to emerging pandemic needs.]
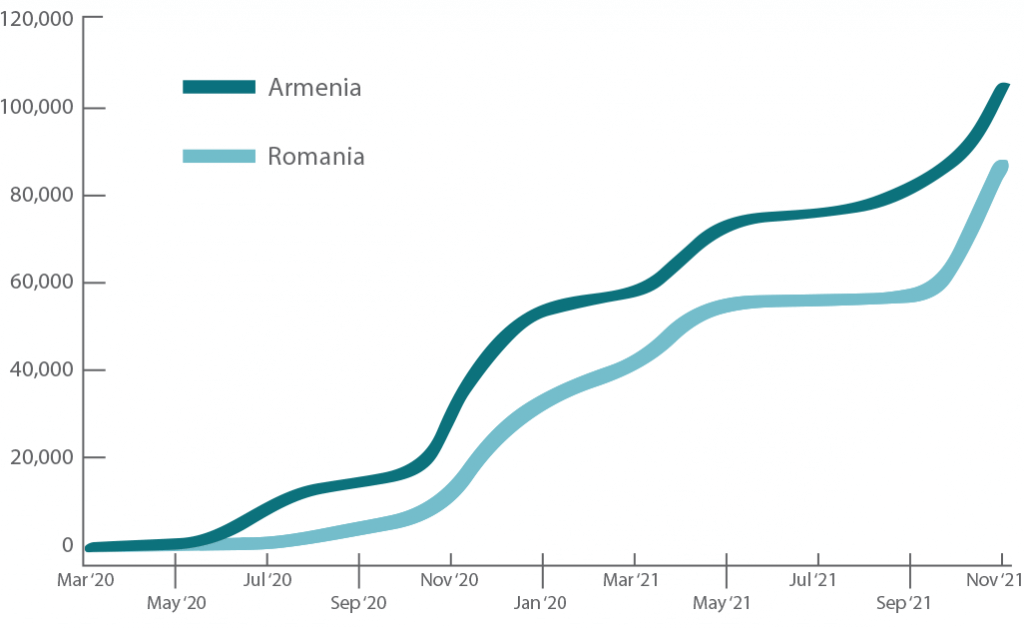
Since the first cases of COVID-19 were reported in December 2019, there have been over 300,000 cases and over 6,000 deaths reported in Armenia. And, as of Oct. 31, 2021, more than 1.6 million cases and more than 46,000 deaths have been reported in Romania (see Figure 1).
The COVID-19 pandemic has challenged health systems around the world, including Armenia and Romania — presenting them with concurrent tasks of reducing transmission, treatment of COVID-19 cases, and ensuring availability of essential non-COVID-19 services.
Social distancing and masking measures have been implemented in many countries, in addition to restrictions on travel, stay-at-home orders, and contact-tracing to isolate cases. Expanding or establishing testing capacity has been necessary to both control the spread of COVID-19 and manage cases in a range of settings, including at home, in first-level facilities, or via hospitalization and intensive care.
Figure 1. Cumulative COVID-19 cases per million in Armenia and Romania
Source: Our World in Data
To meet the multiple demands of detecting and treating COVID-19 cases, while also maintaining other essential health services, health systems have increased health funding, revised purchasing decisions, and implemented emergency measures to adapt service delivery for COVID-19 and non-COVID-19 care.
Increases in fiscal space for health were enabled by borrowing, reallocations within the state budget to the health sector, support from development agencies, and leveraging declarations of states of emergency. More than 40 countries have established funds to support their broader response to the COVID-19 crisis, the majority of which are extra-budgetary — meaning these funds were not initially planned for in their governments’ annual budgets.
The Collectivity project has convened experts from eight countries to comprehensively assess the adjustments in purchasing arrangements as part of the COVID-19 health response and their implications for health system objectives. Purchasing arrangements include the governance structures for purchasing health services, determining what services to buy, from whom to buy, and how to buy (or how services and goods are paid for).
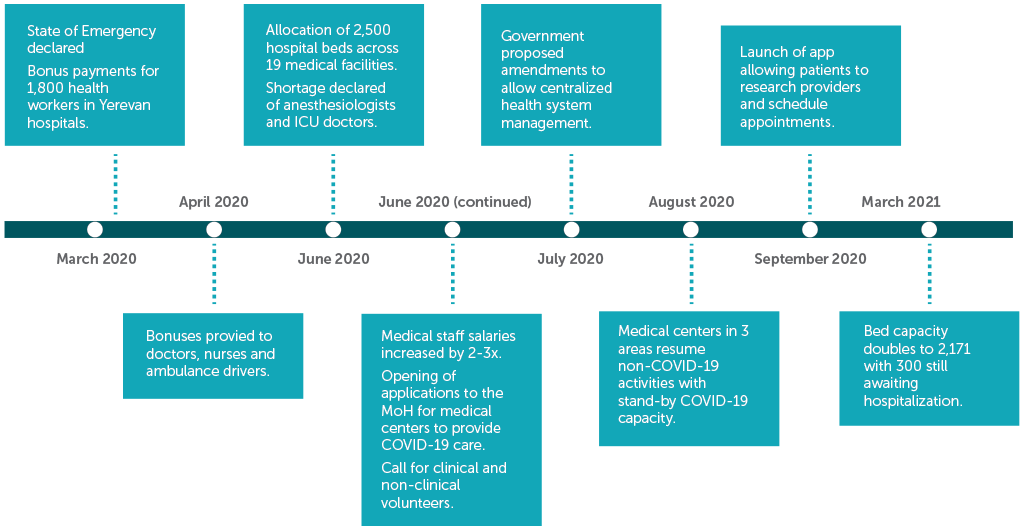
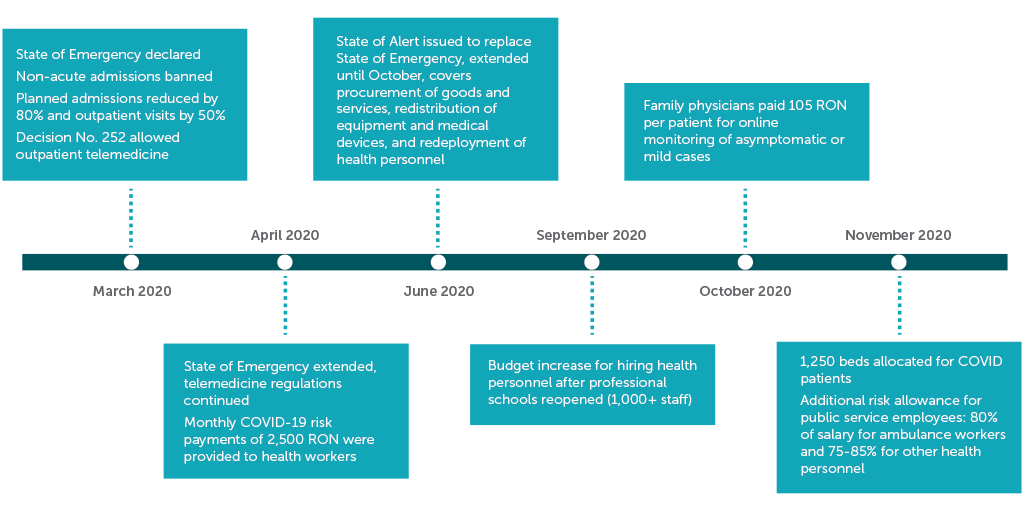
The authors of this blog post conducted an assessment of purchasing changes in response to COVID-19 for Armenia and Romania, presented in Figures 2 and 3, and identified three key lessons on the role of purchasing in pandemic response.
Figure 2. High level health system response measures to COVID-19 in Armenia
Source: Authors’ own design
Figure 3. High level health system response measures to COVID-19 in Romania
Source: Authors’ own design
3. Pandemic-related changes to purchasing arrangements have spurred innovation
With social distancing and restricted movement limiting in-person consultations for primary care and other outpatient services, Armenia and Romania both expanded the state-funded benefits package to include forms of teleconsultation to maintain continuity of services.
In Armenia, telephone consults were increasingly used in lieu of in-person visits for minor COVID-19-related illness and other services.
In Romania, telemedicine visits were added as a reimbursable service to the Framework Contract, a statute governing provider contracting and payment regulations.
The need to track COVID-19 testing, positive cases and case outcomes necessitated the rapid evolution of health information systems. In Armenia, modules to track COVID-19 metrics were quickly developed and deployed as part of the country’s ArMed health information system.
2. Pre-pandemic purchasing arrangements were strategically adapted to respond to emerging pandemic needs
Both countries leveraged existing benefits package structures that guaranteed infectious-disease related services to ensure free COVID-19 services to the entire population.
Health systems in both Armenia and Romania centralized coordination for COVID-19 response, with Romania leveraging existing Ministry of Health authority to manage hospitals and Armenia issuing mandates to coordinate all hospitals providing COVID-19 under the Ministry of Health.
Payment for COVID-19 inpatient care was reimbursed in both countries based on the full cost of providing treatments (including facility costs). Such cost-based mechanisms were more appropriate when there was great uncertainty for providers.
Lessons from the evidence- and goal-driven modifications in purchasing arrangements in both countries can inform approaches to strengthening purchasing toward universal health coverage.
3. Purchasing changes were necessary, buy they can only achieve their intended purposes together with other health system efforts
In response to the COVID-19 pandemic, policy changes related to purchasing governance, what to buy, from whom to buy, and how to buy have been necessary to ensure COVID-19 services are accessible to the entire population and to minimize interruption to non-COVID-19 care.
However, the impact of these measures on accessibility to COVID-19 services were mediated by other complementary factors such as adequate fund flows to scale up service delivery; mobilizing and incentivizing skilled human resources for health, and the reconfiguration of service delivery to facilitate the surge in care for COVID-19.
Other factors outside of the health system may impact availability and quality of services, such as an unstable political environment in Romania. In Armenia, the health system was responding not only to waves of COVID-19 cases but also to regional conflict in late 2020. These additional stressors impact both health system policies related to purchasing for COVID-19 and delivery of essential health services.
The COVID-19 pandemic has challenged health systems to adapt quickly and creatively to provide COVID-19 services to the entire population while maintaining continuity of care in other areas. COVID-19 has tested the flexibility of existing purchasing arrangements and spurred innovation. However, in emergency response and otherwise, purchasing policies can only achieve health system goals along with concurrent and enabling efforts around resource mobilization, service organization, and governance factors outside of the health system.
The insights provided in this series are part of a larger research effort — led by Collectivity country teams — on the strategic purchasing reforms countries developed during the COVID-19 pandemic. Their collective research will culminate in a series of published journal articles. In upcoming posts, we’ll hear from Collectivity teams in Armenia, Romania, Cameroon, Ghana and Ukraine. Click here to learn more on the Collectivity Group on Strategic Purchasing, which aims to contribute to the global knowledge base on strategic purchasing and strengthen the ecosystems that support countries to advance health financing and health system reforms.
Photo © Armine Grigoryan/World Bank
Catch up on the Collectivity Blog Series
- Lessons from the Philippines
- Lessons from Armenia and Romania
- Lessons from Cameroon
- Lessons from Ghana
- Lessons from Ukraine