The journey to strengthening mixed health systems
Building strong, resilient health systems is vital to countries’ efforts to achieve universal health coverage (UHC) and improve health outcomes.
And in many low- and middle-income countries, where people rely on both public and private providers to deliver essential health services, strengthening these mixed health systems requires improving how providers engage with each other (and building better pathways for them to do so).
To that end, we’ve been working with Merck for Mothers to generate more evidence on public-private (mixed) health systems. In our research so far, we’ve learned more about the landscape of global evidence and guidance around public-private sector engagement for health and proposed a public-private sector engagement ecosystem.
We recognize that there is a lot of existing work on mixed health systems focusing on the environmental factors that enable public-private engagement. This engagement is defined as “the deliberate, systematic collaboration of the government and the private health sector according to national health priorities, beyond individual interventions and programmes.”
We’ve gathered and categorized these resources in the Journey Guide for Public-Private Engagement in Health Resource Compendium to facilitate continued use by health system stakeholders. Our contribution to this space is focused on the inner layers of the public-private engagement ecosystem — the structural and engagement factors, which the following approach tries to assess and support.
We’ve also outlined several principles for improving mixed health systems, which — along with learnings from a global evidence review, tacit knowledge, and country expert input — informed our approach. Two principles guided our work, including that:
- Mixed health systems and public-private engagements should be fit-for purpose and responsive to a set of shared, validated country population health needs, demands, and challenges as expressed by the health system actors; and
- As described in a framework for the broader public-private engagement ecosystem, all factors in the public-private engagement ecosystem should be considered in public-private engagement design and implementation, including environmental as well as engagement structural, foundational and operational dimensions.
In this post, we unpack and describe the facilitation approach our team employed over the past two years in India and Kenya to support public-private engagements. The approach is implemented through a trusted broker working side-by-side with public and private sector actors to co-create ways to strengthen and sustain public-private engagements. The approach ensures the process for systems change is country-led and demand-driven, aiming to strengthen the health system to achieve UHC and improved health outcomes.
For this project, we further strengthened the first principle by implementing our support in collaboration with and through local organizations. To do this we identified like-minded local organizations in each country who could take on the role of continuous coaching and mentorship throughout the process and who could be thought partners on the program design and learning. R4D partnered with Insight Health Advisors in Kenya and ACCESS Health International in India. These organizations have ensured that process facilitation approaches are properly tailored to each context and that the evidence used to help inform decision-making processes builds on recent activity and avoids duplication of previous efforts. This work, and we believe any work like this in the future, would not be as successful at mobilizing engagement and motivation from public and private engagement partners without this local credibility and familiarity with the national perspective.
Our approach recognizes the important benefit that a trusted broker brings to public-private engagements. However, we continue to investigate the most sustainable way to design this type of third-party support, acknowledging that not all situations will have the resources to seek out and contract a separate organization to play this facilitative role. Other models could include the public and/or private sector stakeholders performing a local stakeholder mapping to identify if there are already NGO, academic, or community service organizations in their community that would consider taking on this third-party role. Moreover, the tools that have been built from this approach included in the Journey Guide for Public-Private Engagement in Health Resource Compendium were designed so that anyone within a public-private engagement could use them, with or without a trusted broker being available.
Building on these principles, the approach recognizes that mixed health system evolution and strengthening is a complex and challenging process, and countries’ journeys on this path may go in many directions, even backwards at times. So, we designed an approach that would allow stakeholders the flexibility to understand where in the journey they find themselves and help them identify potential pathways that would smooth out that journey at any given point in time; an approach that can be repeated whenever a new system or engagement challenge arises.
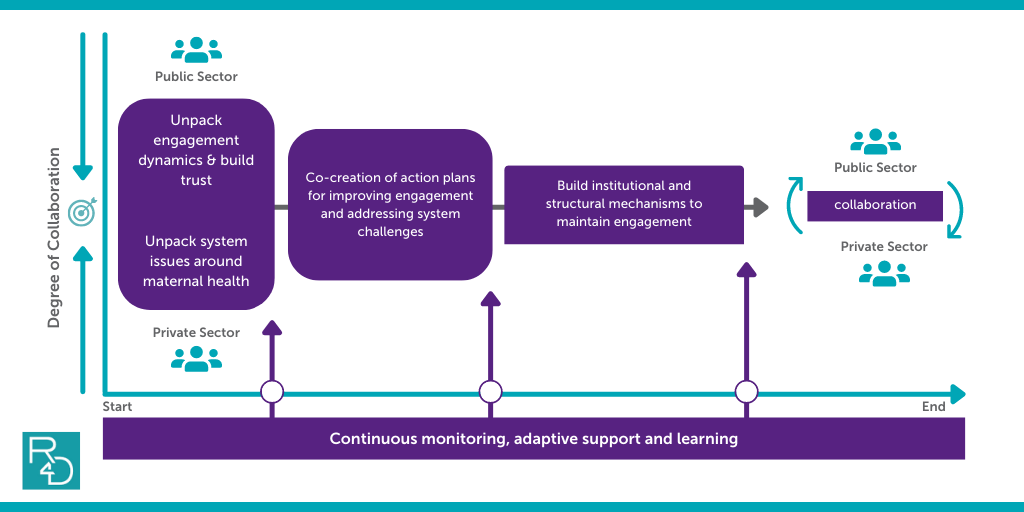
Each step in the approach aims to build trust between stakeholders and create an environment for open and honest engagement, then uses that trust to work together on assessing challenges and designing solutions to address those system and engagement challenges, and then solidifies and sustains that trust through continuous learning, joint implementation, and adaptation based on what is working and not working.
As part of this approach, a trusted broker can facilitate these actions to help stakeholders identify, analyze, and solve problems on their own through collaboration and the use of contextualized evidence.
Figure 1 describes how we applied this approach in collaboration with public and private stakeholders to identify and address system and engagement challenges, including the focus on maternal health challenges, across our two country engagements. R4D, Insight Health Advisors, and ACCESS Health International jointly supported public-private engagements in Kakamega County, Kenya, and Maharashtra, India. These two engagements represented opportunities that demonstrated validated demands and a willingness to engage and reflect on the public-private engagement process from the stakeholders involved.
Figure 1: General SMHS approach to strengthen mixed health systems
The Journey Guide for Public-Private Engagement in Health Resource Compendium describes this process in more detail so that stakeholders interested in adapting this model in Figure 1 can better grasp the content and purpose of each step and make the necessary contextual adaptations for their own public-private engagements. The Journey Guide also provides a detailed review of the Resource Compendium which contains links to additional tools and resources that were used over the last two years. This includes our Co-Creation Workshop Toolkit that provides a facilitation guide, a draft agenda, and an example PowerPoint slide deck that was used to facilitate our workshop in Kenya.
Kenya: How SMHS helped individuals build a team
In Kakamega county, Kenya, health system stakeholders share a concern about stubbornly high maternal mortality rates and the quality of maternal care. When our work began at the county level, there was evidence of ad-hoc communication and interaction between sectors and a motivated but loosely organized private sector. The goals and priorities of these stakeholders focused on setting up a foundation for engagement and tackling broader system challenges that influence these MNCH issues that both sectors shared. Figure 2 provides the overall roadmap of our work in Kakamega.
Figure 2: SMHS approach in Kenya
Unpacking engagement dynamics and system challenges while building trust
Our support to Kakamega started with two sector-specific meetings where Insight Health Advisors facilitated separate discussions with members of the private sector and a team of county health officials to understand and prioritize each group’s main perspectives related to MNCH in Kakamega and obstacles to sustained and efficient engagement across sectors.
Building and using trust across sectors to co-create action plans
These meetings set the foundation for a two-day co-creation workshop where public and private sector stakeholders:
- Validated each other’s perspectives
- Dug deeper into the main challenges they were facing to understand root causes
- Co-developed a set of actions that they could jointly implement to address those issues
As mentioned earlier, the approach that we used to facilitate this workshop is described in our Co-Creation Workshop Toolkit. Insight Health Advisors remained a critical broker, catalyst, and mentor since that workshop to facilitate consistent communication within and across these sector groups, inserting technical support and evidence when relevant, and helping keep momentum on their journey towards achieving their engagement priorities. This continuous support, bolstered by several in-person visits from Insight staff, helped to demonstrate value of each sector’s continued efforts to work together.
Sustaining trust through the ongoing facilitation and strengthening of structural mechanisms
As a result of this process, the Kakamega stakeholders worked on a set of prioritized activities to:
- Support better organization of the private sector and their ability to liaise with the county health management team
- Harmonize approaches to prevent, diagnose, and treat COVID-19 patients, and
- Institutionalize a process for a more inclusive mixed health system approach to health system planning
Most recently, the stakeholders came together with Insight Health Advisors during a county mid-term review meeting and reflected on how they’ve achieved these results so far and what they’d like to do to further build and sustain this engagement in 2021. The inclusion of the private sector association in the mid-term review process and the appointment of a private sector representative in the county M&E committee demonstrates a shift in the way the public sector views, includes, and collaborates with other non-state health actors. In addition, both parties are currently finalizing an MOU to solidify the intentions and framework for better public-private engagements and partnership in the future.
India: Reflecting on progress to date to build a joint vision
In India, many kinds of public-private engagements have been implemented, several of which focus on better partnership to improve maternal mortality across several states. A unique innovation in this space is the joint-accreditation partnership between the Government of Maharashtra and the Federation of Obstetric and Gynecological Societies of India (FOGSI), with technical support from Jhpiego, where government and private sector assessors work together to assure and improve the quality of maternity services in the private sector.
Formalized in 2019, this program called LaQshya-Manyata (L-M) has been a pioneering example of collaboration and alignment of public and private sector efforts to improve maternal health outcomes through ensuring uniformity in quality of care across both sectors. Given that these partners had been working together for some time, the approach to our work in Maharashtra was geared toward supporting stakeholders to pause and reflect on the both foundational and operational engagement factors while also reviewing the environmental factors surrounding L-M and its further integration into the health system.
Unpacking engagement dynamics and system challenges while building trust
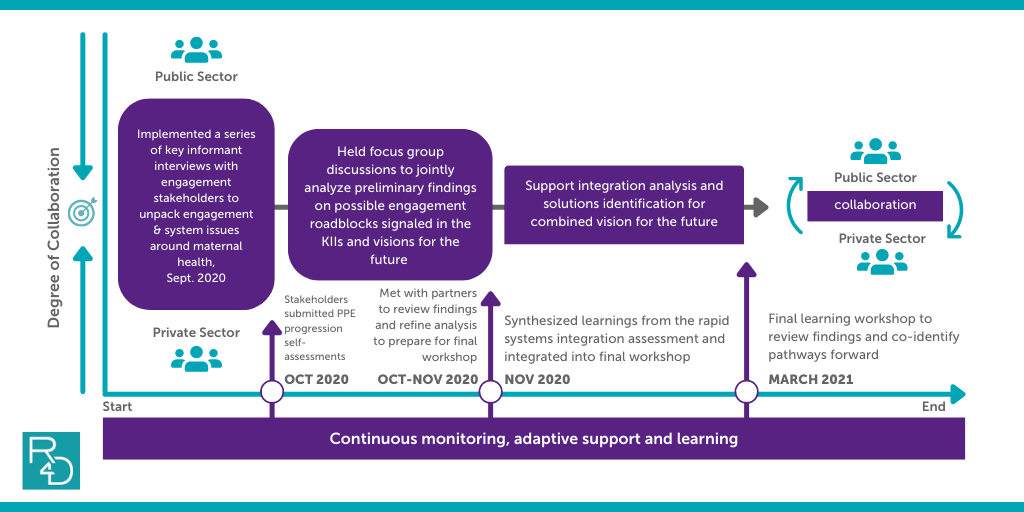
This was a great opportunity for the project to design and test two tools for understanding and improving public-private engagement, the Engagement Factors Self-Assessment Tool and the Rapid Health System Integration Assessment Tool, both of which are included in our The Journey Guide for Public-Private Engagement in Health Resource Compendium. Thus, we adapted the approach outlined in Figure 2 to structure the implementation and use of the tools in a contextually relevant manner, as demonstrated in Figure 3.
Figure 3: SMHS approach in India
We started by first meeting with individual key informants from each of the two primary engagement partners, as well as Jhpiego, to discuss:
- The SMHS public-private engagement ecosystem model
- The importance of the foundational and operational dimensions
- The things that were working well within the engagement and which areas stakeholders would like to focus on strengthening in the coming months.
This step allowed us and our local partner ACCESS Health International to provide a safe space for reflection and analysis within each stakeholder group and get a deeper understanding of how perspectives were aligning or not.
Building and using trust across sectors to prepare for co-creation
To help the public-private engagement actors assess the engagement factors, the facilitation team developed the Engagement Factors Self-Assessment Tool — which is a set of questions that ask respondents to consider the many engagement factors and determine their level of agreement. ACCESS Health disseminated the online questionnaire to L-M actors following the initial key informant discussions and asked them to individually respond to the questions.
Simultaneously, while working directly with partners on the engagement factors, ACCESS Health implemented an assessment of the broader health system using the Rapid Health Systems Integration Tool to analyze what the opportunities and challenges might be for integrating this innovation more deeply into the health system of Maharashtra and the country at large.
In the end, our work intended to culminate in a co-creation workshop with these engagement stakeholders to validate findings from both the self-assessment and the integration assessment. We also planned to outline ideas for how engagement stakeholders would like to collaboratively strengthen and sustain the achievements that this partnership has already produced.
However, due to the challenges of COVID-19, the SMHS project was unable to bring the L-M actors together. Instead, the team packaged the findings and learnings and shared them with L-M actors who may be able to discuss and analyze them further in their own time.
Next steps for this work would include sharing the lessons learned from this engagement with other states across India who may be considering similar joint accreditation approaches or who would like to learn more generally about this PPE ecosystem and how best to assess and strengthen engagement between public and private sector stakeholders.
Where does this work go from here?
While this blog focuses on how we designed and implemented our own aspects of this work in Kenya and India, there is still a need to discuss and learn from what stakeholders within each country did with this approach, which parts resonated with them, and how their individual actions contributed to the progress of public-private engagement and advancement toward UHC in their context.
As with many systems change projects, our work needed to remain flexible and responsive to how the system evolved once our work began. For 2020, this included global health system shocks and changes in health official leadership, among other things, and those exogenous factors required a shift in where this work would go.
In our next blog, our team will outline how we also had to adapt in our role as learning partners within this work and how the adaptation in challenging circumstances may have strengthened our monitoring, evaluation and learning and the approach as a whole in Kenya and India.
The Strengthening Mixed Health Systems project is supported by funding from Merck, through Merck for Mothers, the company’s global initiative to help create a world where no woman has to die while giving life. Merck for Mothers is known as MSD for Mothers outside the United States and Canada.
Photo © Stephan Gladieu/World Bank